By Alexandra Wilson Pecci
Source: Health Leaders Media
For many nurses, leaving high school doesn't mean leaving the bullies behind. Bullying has been called nursing's "dirty little secret," but judging by the numbers, it's hard to believe it could be kept secret at all.
Cheryl Dellasega, PhD, RN, CRNP |
Most women can relate in some way to the 2004 Lindsay Lohan movie Mean Girls, in which her character encounters a group of bullying high school girls who say things like this: "Half the people in this room are mad at me, and the other half only like me because they think I pushed somebody in front a bus."
But while most women can leave memories like this behind when they graduate from high school, for those who enter nursing and become victims of nurse-on-nurse bullying, leaving high school hasn't made the mean girls disappear; they're just wearing scrubs now.
Bullying has been called nursing's "dirty little secret," but judging by the numbers, it's hard to believe it could be kept secret at all.
Twice as many nurses as other Americans have experienced bullying in the workplace. According to study of 612 staff nurses in theJournal of Nursing Management, 67.5% had experienced bullying from their supervisors, while 77.6% had been bullied by their co-workers. Compare that to the 35% of Americans outside healthcare who've reported workplace incivility, says the Workplace Bullying Institute.
Not only is bullying among nurses an issue, it's one that most nurse managers aren't equipped to handle properly, according to Cheryl Dellasega, PhD, RN, CRNP, co-author with Rebecca Volpe of the new book Toxic Nursing: Managing Bullying, Bad Attitudes, and Total Turmoil.
Bullying "is a huge problem now in the workplace," Dellasega tells me. "I think a lot of nurse managers don't get a lot of training in conflict resolution."That's especially true when they have little more management experience than any of their co-workers but were promoted to the role because they have a bachelor's degree and a few extra years of seniority, Dellasega says.
Dellasega's new book is a follow-up her to When Nurses Hurt Nurses: Recognizing and Overcoming the Cycle of Nurse Bullying, and aims to help managers and administrators understand and deal with bullying among their nurses.
In order to write the new book, the authors not only conducted a literature review, but also reviewed hundreds of blogs written by nurses about situations of conflict. By doing so, Dellasega and Volpe were able to identify key themes and scenarios that are common to bullying, as well as which groups of people were commonly involved in bullying.
Finally, the authors interviewed nurse management experts to give insight into dealing with such situations. "There were different pockets of nurses who seemed to be really engaged in the situation, as either a victim of the aggressor," Dellasega says. For example, new nurses are often victims.
"I think that brand new, young nurses [are] sort of the classic targets," Dellasega says. Often, these nurses are idealistic about their work and excited about how they're going to make a difference, but the older, established, more jaded nurses engage in bullying to knock them down a little. In fact, Dellasega says, sometimes the young nurses' preceptors are the ones who are doing the bullying because they feel like the role is a thankless one.
"I know that even…the literature…supports that preceptors often don't feel well prepared to do the job and often don't want to do the job," she says.
Another group of nurses who are often bullied are part-time, agency, or floater nurses who are picked on because they're not part of the regular nurses' clique.
Yes, clique. Dellasega says the regular nurses who are in the clique often make rude or sarcastic comments to or about the new person, or even go so far as not sharing supplies. Even nurses who come in from other floors can be left of out, even though they're just there to help.
Dellasega says that the cliques and bullying in a hospital comes with the same kind of baggage that most of us thought we left behind in high school. But for nurses, there's the added stake of patient safety. Although studies haven't explicitly linked increased bullying to decreased patient safety, research does say that happier nurses do their jobs more effectively. (Conversely, nurse burnout is linked to higher healthcare-associated infection rates).
"It's not a big leap to figure that when you go into work… if there's a toxic environment… you won't be able to give your full attention to patient care," Dellasega says.
Bullying also leads nurses to call in sick more often in order to take mental health days. Abusive behaviors can even cause nurses to develop post-traumatic stress disorder, anxiety, depression, or insomnia, a Joint Commission survey has found. Hospitals can also lose valuable employees to bullying and many nurses have left their jobs because of it.
"Things get to a point where they just can't take it," Dellasega says. Sometimes nurses feel like they're "going into the battle zone every day."
Nurse managers shouldn't let things get to that point. Managing relationships should be day-to-day work, not something that only happens during moments of high tension.
"Don't wait for it to get to the point that there's explosive conflict," Dellasega says.
Just as Dellasega discovered which nurses and situations tend to breed bullying, she and her co-author also discovered which environments are healthy. Bullying is rarer when there is a sense of teamwork, collaboration, and authentic communication with coworkers.
Dellasega says the ideal nurse manager is transparent, letting the staff ask questions and answering honestly, even if the answer is "I don't know, but I'll find out."
Feelings of empowerment are also important to reduce bullying and satisfaction. And upper hospital management should provide appropriate training for new nurse manager about how to effectively and positively deal with bullying.
Finally, Dellasega says nurses managers should monitor their own behavior to ensure that they're not engaged in bullying themselves, even if inadvertently. For example, sighing heavily after someone speaks could be interpreted as negative. Other behaviors to watch out for are favoritism, certain body language, gossiping, and speaking in a raised voice.
"I think nurse manager have to really monitor their own behavior and be cognizant of anything they might do," Dellasega says. "The nurse manager sort of sets the standards.





 determining that Maddie's lungs were immature, rushed her to the NICU. There Maddie's life hung in the balance, and though my wife, Heather, and I longed to care for her ourselves, her condition made it so that we couldn't. We had to trust the NICU nurses to take care of our baby for us, and that was incredibly hard -- especially at night when we went home to catch a few hours sleep.
determining that Maddie's lungs were immature, rushed her to the NICU. There Maddie's life hung in the balance, and though my wife, Heather, and I longed to care for her ourselves, her condition made it so that we couldn't. We had to trust the NICU nurses to take care of our baby for us, and that was incredibly hard -- especially at night when we went home to catch a few hours sleep. named Maddie (also "Bunny" or "Little Mama" as they called her), who was beautiful and strong. I could see that they considered my daughter to be amazing and a gift, and to see others felt about her as I did was incredibly meaningful to me.
named Maddie (also "Bunny" or "Little Mama" as they called her), who was beautiful and strong. I could see that they considered my daughter to be amazing and a gift, and to see others felt about her as I did was incredibly meaningful to me.
 white cap while presiding over the
white cap while presiding over the  Her first opportunity to give an injection involved morphine for a woman with metastatic
Her first opportunity to give an injection involved morphine for a woman with metastatic 

 When you think of a nurse, what’s the first image that comes to mind? Chances are, you think of a woman — and for good reason. The vast majority of professional nurses in the U.S. are white women. In fact, only about six percent of nurses are male and, Considering males make up approximately half of the population and minorities are 30 percent, there’s a major disparity in the profession.
When you think of a nurse, what’s the first image that comes to mind? Chances are, you think of a woman — and for good reason. The vast majority of professional nurses in the U.S. are white women. In fact, only about six percent of nurses are male and, Considering males make up approximately half of the population and minorities are 30 percent, there’s a major disparity in the profession.

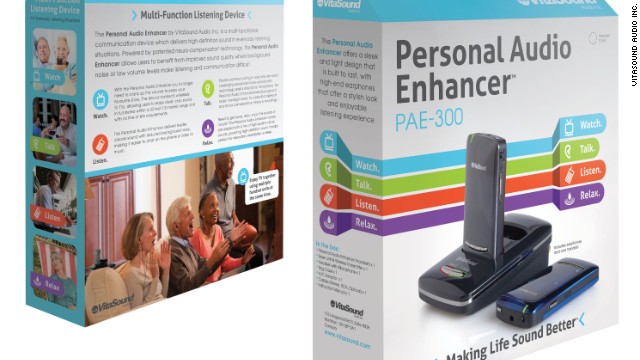
 From "let there be sound" to "let there be light," the next Father's Day gadget is the
From "let there be sound" to "let there be light," the next Father's Day gadget is the 
 The
The  Source:
Source:  As a health care giver, you have a responsibility to ensure that they have adequate knowledge in order to provide competent
As a health care giver, you have a responsibility to ensure that they have adequate knowledge in order to provide competent 


 Source:
Source: 
 By Neal St. Anthony
By Neal St. Anthony






