Teresa Gardner: The roads are narrow and windy curves. So it's not easy to drive the bus.
This is Teresa Gardner's territory. She can't be more than 5-foot-4 but she muscles "the bus" through the hollers, deaf to the complaints, of a 13-year-old Winnebago that's left its best miles behind it.
Teresa Gardner: Having problems seeing here.
Scott Pelley: You really can't see.
The wipers are nearly shot and the defroster's out cold.
Scott Pelley: There you go, you can see a little better now. I understand there's a hole in the floorboard here somewhere?
Teresa Gardner: Yes, it's right over there so don't get in that area.
The old truck may be a ruin but like most RVs it's pretty good at discovering America. Gardner and her partner, Paula Meade, are nurse practitioners aboard the Health Wagon, a charity that puts free health care on the road.
[How many patients do we have on the schedule today?
He was going to see what he can free up for us.]
The Health Wagon pulls up in parking lots across six counties in southwestern Virginia.
[Y'all come on in out of the rain.]
It's not long before the waiting room is packed.
[Hello Mr. Hank, how you doing?]
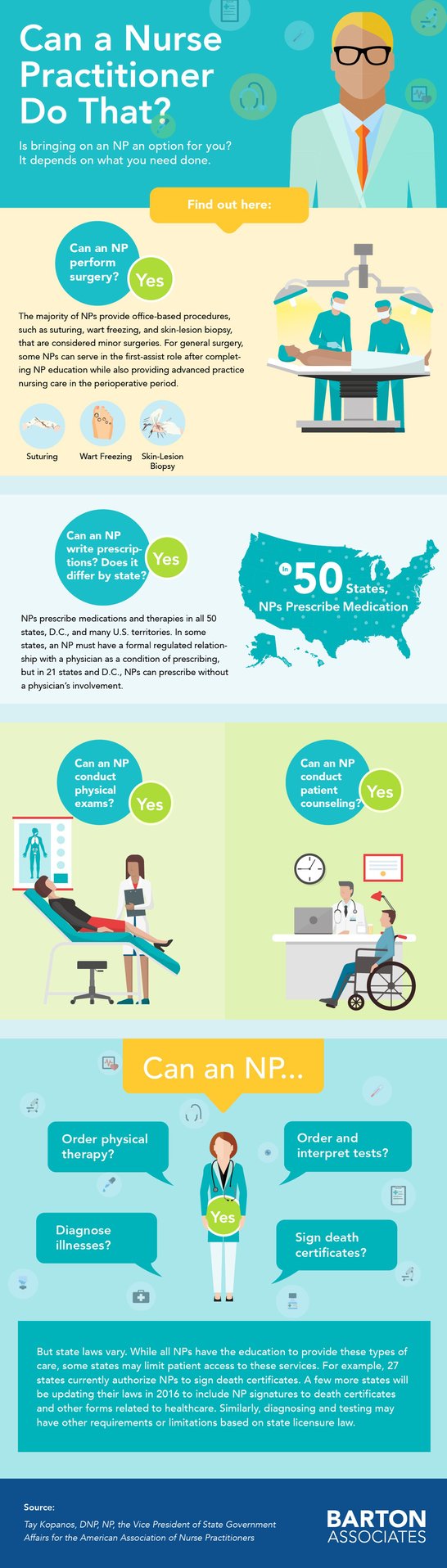
And two exam rooms are full. With advanced degrees in nursing, Gardner and Meade are allowed to diagnose illnesses, write prescriptions order tests and X-rays.
[Stick it out, ahhh.]
On average there are 20 patients a day, that's recently up by 70 percent. The Health Wagon is a small operation that started back in 1980. It runs mostly on federal grants and corporate and private donations.
[Blood pressure a bit high before?
Just when I get aggravated.]
Scott Pelley: Who are these people who come into the van?
Paula Meade: They are people that are in desperate need. They have no insurance and they usually wait, we say, until they are train wrecks. Their blood pressures come in emergency levels. We have blood sugars come in 500, 600s because they can't afford their insulin.
Scott Pelley: But why do they not see a doctor or a nurse before they become, as you call it, train wrecks?
Paula Meade: Because they don't have any money. They don't have money to pay for labs. They don't have money to go to an ER and these are very proud people. They, you know, you go to the ER, you get a $3,500 bill. And then what do you do? You're given a prescription, you can't fill it. That's why they're train wrecks. They have nowhere else to go.
Glenda Moore had nowhere to go but the ER when the pain in her leg became unbearable. Her job at McDonald's, making biscuits, didn't include insurance that she could afford.
Glenda Moore: The only doctor that would see me-- you had to have $114 upfront just to be seen.
Scott Pelley: What does $114 mean to your monthly budget?
Glenda Moore: Oh my gosh. That's half of my weekly pay. I make $7.80 an hour. My paycheck was about after taxes about $475 every two weeks.
The pain was from a blood clot. She needed Lovenox, a clot buster that cost about $500 for a full treatment.
[Paula Meade: Was she on Lovenox when she was discharged from the hospital?]
Paula Meade got the call from the ER, which didn't want to bear the cost. The Health Wagon had the drug for free and there was no charge for some stern medical advice.
Paula Meade: You are going to die if you don't quit smoking and it could be within a week. You need to stop now! OK?
She took the advice to stop smoking and took Lovenox but one day she felt so bad she went back to the ER.
Glenda Moore: And they did a CAT Scan and an X-ray and found the blood clot had went to my lung. But they also saw another mass on my lung. And then transported me to a bigger hospital. They found the lesions in my brain, so I was diagnosed with stage IV lung cancer and brain cancer.
Scott Pelley: What are the doctors telling you?
Glenda Moore: I start my treatment on Monday, the brain radiation, and he seemed very, I mean he seemed optimistic.
Scott Pelley: Are you hopeful?
Glenda Moore: I am. I have been. I don't know, I just feel very hopeful.
Hope, especially when the odds are long, has always been essential to survival in Appalachia. The recovery from the Great Recession hasn't arrived. In coal these days they just take the top of the mountain and you don't need many men for that. Around here a thousand were laid off in the last two years. Twelve percent of the folks don't have enough to eat. And we met them waiting for their number at Zion Family Ministries Church where a charity called Feeding America was handing out just enough to get through a week -- if you stretch. 1,654 lined up -- a parking lot of possibilities for the Health Wagon, Gardner and Meade. They've known these people and each other most their lives.
Scott Pelley: You've been together since 8th grade?
Paula Meade: Eighth grade. Yes.
Scott Pelley: Why do you do this work?
Paula Meade: Because somebody has to. You know, there's people here, you know, we always, we had dreams. We wanted to move away from here. We all, you know, we did. And then we come back and we saw the need. And actually there's a vulnerable population here that's different from the rest of America. I mean there are people, you can replicate this. But we're kind of forgotten. There's no one here to take care of 'em but us.
These patients would be taken care of in the 26 states that expanded Medicaid under Obamacare. The federal government pays the extra cost to the states for three years but Virginia and the others that opted out fear that the cost in the future could bankrupt them. So the health wagon patients we met have fallen through this untended gap.
[Do you have insurance?
No ma'am.]
Scott Pelley: Have any of you tried to sign up for the president's health insurance plan?
Voices: No--
Scott Pelley: Why not?
Brittany Phipps: I can't afford it.
Sissy Cantrell: I can't either.
Sissy Cantrell was laid off from a head start center. She's been suffering from migraines and seizures.
[I cry for no reason at all. OK.
Have you been seeing a counselor?
No.
OK.]
She came away from the Health Wagon with medication.
[I did want to ask you....]
Brittany Phipps works more than 50 hours a week, but that's two part-time jobs so there's no insurance for her diabetes.
Scott Pelley: So you're getting your insulin through the Health Wagon?
Brittany Phipps: I am now. Yeah.
Scott Pelley: And if that wasn't available, where would you get the insulin?
Brittany Phipps: I don't know.
Walter Laney's diabetes blinded him in one eye and threatens the other. The Health Wagon stabilized him and set him up with a specialist.
[Hey Walter, this is Dr. Isaacs, how's it going?
Pretty good.
How've you're sugars been?
OK.]
Walter Laney: They got my blood sugars back under control. Before this year, I was in the hospital three, four times and this year, I ain't been in none since I've been seeing them. If it hadn't a been for them, I don't think I'd be here today.
Outside the church where they were handing out food we met Dr. Joe Smiddy, a lung specialist who's the Health Wagon's volunteer medical director.
Joe Smiddy: This is a Third World country of diabetes, hypertension, lung cancer, and COPD.
Dr. Smiddy drives a second Health Wagon, a tractor-trailer X-ray lab.
Scott Pelley: I guess they taught you something about radiology and all of that in medical school. Did they teach you how to drive an 18-wheeler?
Joe Smiddy: I did have to go to tractor-trailer school. And it took a long time.
Scott Pelley: Was that harder than medical school in some ways?
Joe Smiddy: It was very difficult to get anyone to insure a doctor to drive a tractor-trailer. The insurance companies didn't believe me.
His X-ray screen is a window on chronic, untreated disease including black lung from the mines.
Joe Smiddy: We've seen coal workers pneumoconiosis, emphysema, COPD, enlarged hearts. There's 15 of the 26 had significant abnormalities here today.
Scott Pelley: Just today?
Joe Smiddy: Just today.
Scott Pelley: But when they leave your Health Wagon, they still don't have health insurance. How do they get treated for these things that you're finding?
Joe Smiddy: We negotiate. We can talk to the hospital system. We don't leave any patient unattended. We raise money for them.
Scott Pelley: You find a way.
Joe Smiddy: We will find a way.
They found a way to get Glenda Moore radiation for her brain cancer. But she'd been a smoker for 25 years. And she died three months after our interview.
Scott Pelley: You don't like this idea of receiving charity?
Glenda Moore: No. Oh, I hate it. My dad was in the military. And when he was diagnosed with cancer, he was taken care of. And I don't know, I just always assumed, you know, that's how it would work.
Scott Pelley: Do you think things would've been different if you'd had an opportunity to go to a doctor more often?
Glenda Moore: Oh, definitely. I know it would be different.
The outreach to all the people like Glenda Moore costs the Health Wagon about a million and a half dollars a year, a third of that is from those federal grants, and the rest from donations. Doctors volunteer and pharmaceutical companies donate drugs. But when we were with them...
[We got no electricity on the health side.]
...they sure could have used a new truck battery.
[There goes.Yay! ]
Teresa Gardner: Can we give you all a free flu shot for helping us?
Man: Need a free flu shot, Beaver? Nope. Ok.
Teresa Gardner and Paula Meade apply for grants. And travel to churches praying for donations and passing the plate.
Scott Pelley: Are there days you say to yourself, "I can't do this anymore."
Paula Meade: Oh, every day. Not every day. I shouldn't say every day. There are a lot of days you get frustrated because we're writing grants till 10:00 at night. We're begging for money. And you're almost in tears because we're like, "OK, what are we gonna do," because I've got a family too. It gets frustrating, it gets hard.
Scott Pelley: It's enough to wear you out, Teresa.
Teresa Gardner: We're pretty beat down by the end of the day on most days really. But we do get more out of it then we ever give.
Paula Meade: When you look at it practically, you think, "What in the world am I thinking?" But then I have that one patient that may come in and say, "Couldn't bring you anything, can't pay anything but here's a quilt I wanna give you." And I mean when they do that and they're so heartfelt and you just-- and they put their arms around you, "I don't know what I'd do without you..."
[You're doing a lot better.]
Paula Meade: It lets you think, "OK, I was put here for a purpose."
Teresa Gardner: And you can do it another day.
[You're a blessing to us.
Well thank you all. You're blessing us. ]
Teresa Gardner: It's them and that's what touches our heart.
This week in Virginia, there is a crisis at the capital where the new Democratic governor is demanding Medicaid expansion from the Republican House. But neither side will budge and now there's a threat of a government shutdown in that state. There's no shutting down the Health Wagon though. Gardner and Meade have raised money for a new truck and they hope to get it on the road in the spring.
Source: 60 Minutes


 The
The  As a Nurse Practitioner, the state you live and work in has different laws and regulations that impact your practice. There are 3 different authorization categories -- Full Practice, Reduced Practice, and Restricted Practice. Here are the details and states for each practice.
As a Nurse Practitioner, the state you live and work in has different laws and regulations that impact your practice. There are 3 different authorization categories -- Full Practice, Reduced Practice, and Restricted Practice. Here are the details and states for each practice. Think you need to
Think you need to