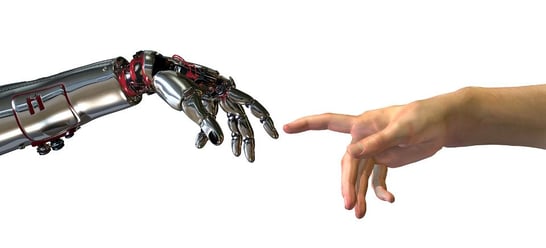
Although technology could never replace compassion and human interaction, it can significantly improve and streamline processes and procedures to ensure patients receive the best quality care. Healthcare technologies can make patient care better, easier, and more efficient, especially with a large patient load. Here are some current healthcare technologies you should get to know to help better provide Nursing care to your patients.
Telehealth
Telehealth has become a buzzworthy topic in the healthcare community. Telehealth has been gaining popularity for years but was significantly accelerated due to the COVID-19 pandemic. Telehealth services enable Nurses to interact with patients, assess their symptoms and conditions, provide instructions for care, and offer support, all without being physically present with their patients.
One of the many benefits of telehealth is it can enhance access to healthcare for individuals living in remote or rural communities or those with limited mobility. It also significantly reduces travel time and patient expenses, improves care coordination, and allows Nurses to reach a larger patient population.
Wearable Medical Devices
Wearable medical devices offer Nurses new tools to enhance patient care and monitoring. These devices can wirelessly transmit patient information such as vital signs, blood sugars, and ECG patterns to Nurses to quickly analyze and interpret the data. Wearable medical devices offer valuable data in real-time, enhance the patient experience, and help Nurses deliver quality patient care to all patients regardless of their geographical location.
Electronic Health Records
Electronic Health Records (EHRs) have revolutionized how Nurses manage patient information and care. EHRs are digital versions of patient medical records containing comprehensive information about medical and health history, current diagnoses, medications, treatments, and other relevant medical data to help you provide better patient care.
EHRs have streamlined documentation for Nurses to document patient information which, as a result, reduces the need for physical storage space, eliminates handwriting legibility issues, and provides a structured documentation format.
Point of Care Technology
Point-of-care technology (POCT) refers to medical devices and technologies that enable Nurses to access and utilize patient information and perform diagnostic testing while providing care directly at the bedside or point of care. Point-of-care technologies used by Nurses can include mobile devices like smartphones and tablets that allow access to EHRs, medication databases, clinical references, and communication platforms to communicate with healthcare team members.
Nurses often utilize other hand health point-of-care technologies like digital thermometers, pulse oximeters, portable EKG machines, portable ultrasound, and blood sugar monitors. POCT improves efficiency, accuracy, and patient outcomes by enabling Nurses to access important information, perform testing and get rapid results, and deliver care directly at the bedside, which promotes patient engagement.
Patient Portals
Patient portals are online platforms that allow patients to access their health information, communicate with healthcare providers, and engage in their care. Nurses can use patient portals to educate patients, communicate with patients, and coordinate care. We can foster a collaborative and patient-centered approach when Nurses utilize patient portals and other mobile health apps to connect with patients.
The Impact of Technology on the Nursing Profession
As technological advancements evolve, Nurses must continuously learn to adapt and acquire new skills. There are numerous advantages for Nurses who utilize healthcare technology, including faster communication, increased efficiency, improved access to patient information, and reduced Nurse burnout. Nurses who stay informed and embrace developing technology can help lead the way toward a brighter future for the Nursing profession.



 With technology consistently evolving, Nurses will see an influx of new advancements throughout the next couple of years. Nurses will have the opportunit
With technology consistently evolving, Nurses will see an influx of new advancements throughout the next couple of years. Nurses will have the opportunit
 Technology continues to make strides in both our professional and personal lives. This article is about a robot that’s being tested to deliver medication to chemo patients, thus eliminating the step of having to wait in line for medication after a very lengthy day of chemo. This is a new technology being tested at Dana Farber Cancer Institute and patients are enthusiastic about it.
Technology continues to make strides in both our professional and personal lives. This article is about a robot that’s being tested to deliver medication to chemo patients, thus eliminating the step of having to wait in line for medication after a very lengthy day of chemo. This is a new technology being tested at Dana Farber Cancer Institute and patients are enthusiastic about it.
 Brain training with virtual reality systems and robotic exoskeletons are helping paraplegic patients regain some sensations and possibly mobility. Brain-machine interface is changing diagnoses from complete to partial paralysis.
Brain training with virtual reality systems and robotic exoskeletons are helping paraplegic patients regain some sensations and possibly mobility. Brain-machine interface is changing diagnoses from complete to partial paralysis.
 3D printing has come to the rescue of severe cases of a childhood disease in which the windpipe is softened, leading to collapse of the airway and breathing failure. Previously lacking any adequate intervention, tracheobronchomalacia has found an innovative fix in three babies whose condition presented them with little chance of reaching young childhood.
3D printing has come to the rescue of severe cases of a childhood disease in which the windpipe is softened, leading to collapse of the airway and breathing failure. Previously lacking any adequate intervention, tracheobronchomalacia has found an innovative fix in three babies whose condition presented them with little chance of reaching young childhood. Medication errors continue to plague the clinical community and even rare cases of mistakes can make a big splash in the news. And for a good reason: we all expect to be treated than harmed when receiving medical care. A new device is currently in the third round of pilot testing, including at major retail pharmacies and Purdue University, that may help avoid prescription errors altogether. The IdentRx system from PerceptiMed, a Mountain View, California firm, optically analyzes every single pill that will be given to a patient to make sure it precisely matches each prescription.
Medication errors continue to plague the clinical community and even rare cases of mistakes can make a big splash in the news. And for a good reason: we all expect to be treated than harmed when receiving medical care. A new device is currently in the third round of pilot testing, including at major retail pharmacies and Purdue University, that may help avoid prescription errors altogether. The IdentRx system from PerceptiMed, a Mountain View, California firm, optically analyzes every single pill that will be given to a patient to make sure it precisely matches each prescription.
