 As a medical professional, you are all too aware of the use of antibiotics and how effective they are for treating a myriad of infections. They have helped relieve countless maladies for people all over the world. We want to share this article with you and we welcome your thoughts and experiences about what’s happening regarding antibiotics not working for some of your patients.
As a medical professional, you are all too aware of the use of antibiotics and how effective they are for treating a myriad of infections. They have helped relieve countless maladies for people all over the world. We want to share this article with you and we welcome your thoughts and experiences about what’s happening regarding antibiotics not working for some of your patients.
In early April, experts at a military lab outside Washington intensified their search for evidence that a dangerous new biological threat had penetrated the nation’s borders.
They didn’t have to hunt long before they found it.
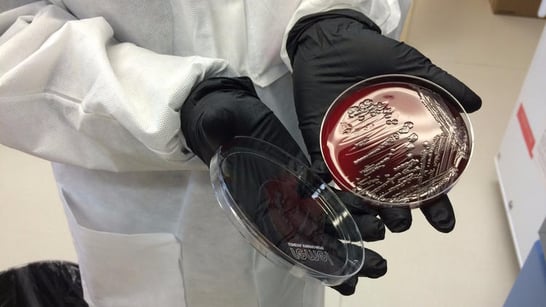
On May 18, a team working at the Walter Reed Army Institute of Research here had its first look at a sample of the bacterium Escherichia coli, taken from a 49-year-old woman in Pennsylvania. She had a urinary tract infection with a disconcerting knack for surviving the assaults of antibiotic medications. Her sample was one of six from across the country delivered to the lab of microbiologist Patrick McGann.
Within hours, a preliminary analysis deepened concern at the lab. Over the next several days, more sophisticated genetic sleuthing confirmed McGann’s worst fears.
There, in the bacterium’s DNA, was a gene dubbed mcr-1. Its presence made the pathogen impervious to the venerable antibiotic colistin.
"We’re seeing more drug-resistant infections. And people will die."
More ominously, the gene’s presence on a plasmid — a tiny mobile loop of DNA that can be readily snapped off and attached to other bacteria — suggested that it could readily jump to other E. coli bacteria, or to entirely different forms of disease-causing organisms. That would make them impervious to colistin as well.
It was a milestone public health officials have been anticipating for years. In a steady march, disease-causing microbes have evolved ways to evade the bulwark of medications used to treat bacterial infections. For a variety of those illnesses, only colistin continued to work every time. Now this last line of defense had been breached as well.
A second U.S. case of E. coli with the mcr-1 resistance gene was reported this week in the journal Antimicrobial Agents and Chemotherapy. Researchers are still working to determine whether it, or any of 18 other samples from around the world, contained the gene on an easy-to-spread plasmid.
Related Article: Kids Prescribed Antibiotics Twice As Often As Needed, Study Finds
Like this article? Click below to receive our FREE bi-weekly newsletter full of interesting articles like this one!



