The healthcare landscape is evolving rapidly, and at the forefront of this transformation is the rise of Nurse Practitioners (NPs). With a growing shortage of physicians, an aging population, and increased demand for accessible care, NPs have become an integral part of the healthcare system. But with this rise, a question often comes up: Are Nurse Practitioners replacing Doctors? Let’s take a closer look at the role of NPs, their impact on healthcare, and whether they are a threat to the traditional role of Physicians.
Who Are Nurse Practitioners?
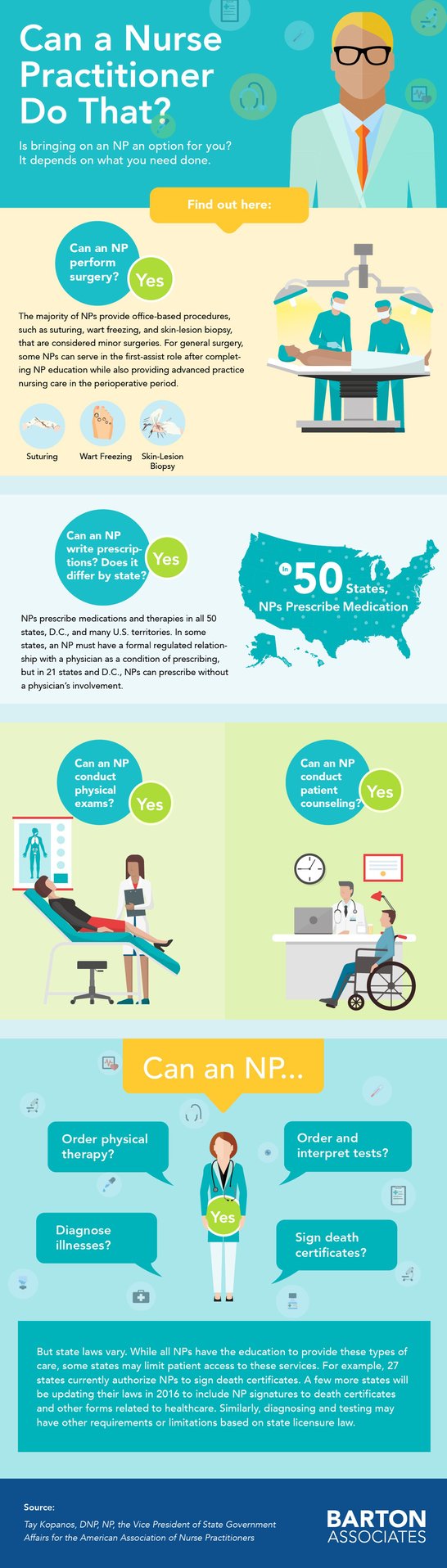
Nurse Practitioners are Advanced Practice Registered Nurses (APRNs) who have completed additional education and training beyond their Registered Nurse (RN) licensure. Most NPs hold a master’s or doctoral degree and are trained to diagnose illnesses, prescribe medications, and provide treatment. They often specialize in areas such as family medicine, pediatrics, women’s health, or geriatrics.
What sets NPs apart from RNs is their expanded scope of practice, which allows them to deliver primary, acute, and specialty care independently or in collaboration with a Physician, depending on the state in which they practice.
The Impact of NPs on Healthcare
Increased Access to Care One of the biggest impacts of the rise of Nurse Practitioners is improved access to healthcare, especially in underserved or rural areas. NPs are often more likely to work in these regions, helping to fill gaps in care where Physicians may be scarce. As the shortage of Doctors continues, particularly in primary care, Nurse Practitioners provide a much-needed solution, offering care to patients who might otherwise have difficulty accessing services.
Cost-Effective Care Nurse Practitioners provide high-quality care at a lower cost than Physicians, helping to reduce healthcare expenses for both patients and healthcare systems. Studies have shown, the care provided by NPs is just as effective as that delivered by Doctors for a wide range of primary and chronic conditions. With healthcare costs skyrocketing, Nurse Practitioners play a crucial role in containing costs while maintaining patient satisfaction.
Patient-Centered Approach One of the hallmarks of NP practice is a focus on patient-centered care. NPs are known for spending more time with patients, taking a holistic approach to health, and emphasizing education and prevention. This personalized care often results in better patient outcomes and higher satisfaction rates, making NPs a popular choice for many patients.
Alleviating Physician Burnout As Physician burnout continues to be a major concern in healthcare, Nurse Practitioners help alleviate the pressure by sharing the patient load. NPs can handle many of the same responsibilities as Doctors in primary and specialty care settings, allowing Physicians to focus on more complex cases. This collaborative approach benefits both healthcare providers and patients, as it leads to better work-life balance for Doctors and more comprehensive care for patients.
Are Nurse Practitioners Replacing Doctors?
While Nurse Practitioners are playing a larger role in healthcare, they are not "replacing" Doctors. Instead, they are filling a critical need, especially in primary care. The role of a Doctor remains essential, particularly in specialized fields like surgery, oncology, and complex diagnostics, where advanced medical training is required.
The relationship between NPs and Physicians is increasingly seen as complementary rather than competitive. In many settings, NPs and Doctors work together to provide high-quality care, leveraging each other’s strengths. Collaborative care models, where Physicians and NPs work in tandem, are becoming more common, leading to better patient outcomes.
State Regulations and Scope of Practice
One key factor in the rise of Nurse Practitioners is the expansion of their scope of practice in many states. Currently, 27 states and Washington, D.C., allow full practice authority for NPs, meaning they can diagnose, treat, and prescribe medications without Physician oversight. Other states have more restrictive regulations, requiring some level of Physician supervision or collaboration.
The trend toward granting NPs full practice authority is likely to continue as healthcare systems seek more flexible solutions to meet patient demand. This shift doesn't diminish the importance of Physicians but instead broadens the range of options for patients to receive timely, effective care.
The Future of Healthcare: A Team Approach
The rise of Nurse Practitioners is a positive development for healthcare. With their ability to provide quality, cost-effective care, NPs are helping to bridge the gaps in access and affordability. However, the future of healthcare isn’t about choosing between Doctors and NPs—it’s about collaboration. By working together, Doctors and Nurse Practitioners can create a more efficient, patient-centered healthcare system that meets the needs of a diverse and aging population.
In conclusion, while Nurse Practitioners are stepping into roles that were once dominated by Physicians, they are not replacing Doctors. Instead, they are enhancing the healthcare system by providing accessible, personalized care, helping to alleviate Physician shortages, and improving outcomes for patients. The future of healthcare lies in teamwork, with NPs and Physicians working side by side to deliver the best care possible.


 Think you need to
Think you need to