
The School Nurse shortage is not a new issue. The pandemic highlighted the importance of having School Nurses. As schools across the nation open back up,
concerns are again rising.
The US Centers for Disease Control and Prevention (CDC) recommends schools have one full-time Nurse for every 750 students.
The latest data from a study, published in the Journal of School Nursing in 2018, found approximately 39% of schools employ full-time Nurses and about 35% employ part-time School Nurses, while 25% do not employ School Nurses.
With out School Nurses, teachers and staff with no medical training would be responsible for providing care such as dispensing medication, managing allergies and asthma, and monitoring blood glucose levels.
Not only are School Nurses responsible for providing care, they also play a vital role in the management of COVID-19 safety protocols and updating staff and parents.
According to a survey from the National Association of School Nurses (NASN), 78% of School Nurses say they took time to review data to see new trends in COVID infections. The survey shows 43% of Nurses spent time updating and developing school health policies and nearly half said they were spending time answering phone calls from parents and the community.
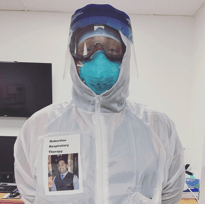
“I spend most of my day dressed up as a ghostbuster in personal protective equipment,” Rhonda Cranford, a School Nurse at Northside Elementary with 34 years of experience, shared. “I’m answering the phone constantly with questions regarding isolation and quarantine. I spend hours documenting and sending emails. Ninety-five percent of my day is consumed by COVID activities.”
Many schools have a tight budget and can lack the funding needed to hire a School Nurse.
Laurie G. Combe, NASN President said, “When budgets are tight, administrators make decisions to hire Teachers over Nurses, but what many administrators don’t understand is that having a Nurse on staff can actually save dollars."
A glimmer of hope arose in May when the Biden administration announced the American Rescue Plan. The Plan includes dedicated funding of at least $500 million to hire School Nurses to help schools safely reopen and remain open for in-person instruction.
It’s important to remember there is a Nursing shortage across the country. School districts are competing against healthcare organizations for Nursing applicants where wages in hospitals and other settings tend to pay more.
Between the Delta variant, mask protocols, and vaccine mandates, schools need Nurses now more than ever.



 In the wake of the COVID-19 pandemic, higher education is seeing a rise in demand for health and medical education.
In the wake of the COVID-19 pandemic, higher education is seeing a rise in demand for health and medical education.
 Nurses are a critical part of healthcare and make up the
Nurses are a critical part of healthcare and make up the  More Universities and Colleges have considered hiring Chief Health Officers (CHO) as the COVID-19 pandemic rages on. Some responsibilities of the CHO would be to lead campus health and safety measures, create connections with state and local hospitals, and be the voice of information to students, employees and parents.
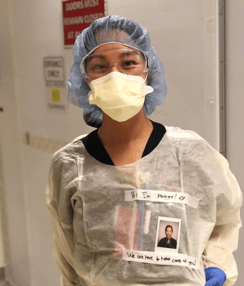
More Universities and Colleges have considered hiring Chief Health Officers (CHO) as the COVID-19 pandemic rages on. Some responsibilities of the CHO would be to lead campus health and safety measures, create connections with state and local hospitals, and be the voice of information to students, employees and parents. An estimated 4%, or about 150,000, Nurses in the U.S. are Filipino, but comprise nearly a third of Registered Nurse deaths due to COVID-19.
An estimated 4%, or about 150,000, Nurses in the U.S. are Filipino, but comprise nearly a third of Registered Nurse deaths due to COVID-19. School Nurses have become the main point of contact for any and all things COVID-19 related. They are a key component in making sure schools stay open.
School Nurses have become the main point of contact for any and all things COVID-19 related. They are a key component in making sure schools stay open.


 COVID-19 has shone a light on how
COVID-19 has shone a light on how Many Nurses and Doctors said in interviews with
Many Nurses and Doctors said in interviews with