Nearly seven million hospitalized patients each year acquire infections while being treated for other conditions. The culprit, according to a study published in the American Journal of Infection Control, is nurse burnout and has been linked to higher rates of hospital-acquired infections (HAIs).
“There is a tendency for nurses to get tired and want to take a break when they are taking on a heavier than normal load of patients, so they may cut corners to get work done,” says Cheryl Wagner, Ph.D., MSN/MBA, RN, associate dean of graduate nursing programs at American Sentinel University. “Nurses may ‘forget’ proper nursing care, such as dressing changes and emptying of drainage bags, or not pay attention to details such as hand washing and careful handling of contaminated articles, and this can be a major cause of hospital-acquired infections.”
Nurse burnout is that feeling of emotional exhaustion and disillusionment nurses feel about their current job that can creep up when working with heavy patient loads and under stress. These problems affect nurses both personally and professionally, and it may affect their patients as well.
A team of researchers at the University of Pennsylvania used a survey tool called the Maslach Burnout Inventory to analyze nurses’ job-related attitudes. It then compared a hospital’s percentage of burnout nurses to its rates of catheter associated urinary tract infections (CAUTIs) and surgical site infections (SSIs).
The researchers found that every 10 percent increase in the number of high-burnout nurses correlated with one additional CAUTI and two additional SSIs per 1,000 patients annually.
At first glance, this might not seem like a big deal, but according to the Association for Professionals in Infection Control (APIC), using the per-patient average costs associated with CAUTIs ($749 to $832 each) and SSIs ($11,087 to $29,443 each), researchers estimate that if nurse burnout rates could be reduced to 10 percent from an average of 30 percent, Pennsylvania hospitals could prevent an estimated 4,160 infections annually with an associated savings of $41M.
Impact of Work Environment
A study by the Agency for Healthcare Research and Quality (AHRQ) offers evidence that nurse-to-patient staff ratios has been linked with patient outcomes. It seems rather clear-cut that, from time constraints alone, fewer caregivers would translate into a lower standard of care. But this study goes a step further, suggesting the issue is not simply the number of nurses on staff, but the quality of the work environment.
When nurses feel there is a lack of teamwork, or that management’s values conflict with their own – putting financial concerns ahead of patient safety, for instance – stress can build up to the point that some nurses simply detach from their work.
Because Medicare and some private insurers are no longer reimbursing for CAUTIs and SSIs, it only makes sense that hospitals would do everything possible to eliminate these adverse events. That includes not only encouraging nurses to adhere to infection control practice guidelines, but also to improve the work environment as well.
“By reducing nurse burnout, we can improve the well-being of nurses while improving the quality of patient care,” says Dr. Wagner.
Dr. Wagner notes that one common method to reduce nurse burnout is to make sure that staff has adequate time for rest periods.
“This means ensuring that nurses get their days off and are not asked to work additional hours due to shortages, or that they get the regular breaks that they need throughout their workday,” she adds.
More importantly, Dr. Wagner believes that evidence-based staffing standards play an important role in reducing nurse burnout.
“Evidence-based staffing standards will help organizations to staff adequately and avoid nurse burn out, but this evidence must be brought forward by highly educated nurses so that it can have the proper impact.”
Dr. Wagner points out that just complaining about poor staffing does nothing to alleviate the situation and that the evidence needs to be presented by well-educated nurses in formal proposals to administrators.
The needs of the patients grow more complex in today’s health care environment and if a nurse is to be able to handle a multitude of patients with varying maladies, then they need to have the education that will give them the best abilities to improve patient outcomes.
Infection Control Resources
Dr. Wagner reminds nurses that there are simple steps they can take to help reduce the incidence of HAIs. Hand washing is at the top of the list. Other preventive measures bring a nurse’s role as patient advocate into play.
Dr. Wagner recommends that nurses conduct daily reviews of all their patients who have catheters and advocate for the removal of those that are no longer necessary.
Research shows that ‘forgotten catheters’ are often inappropriate catheters, so it’s important that nurses don’t assume that physicians are always aware of a patient’s catheter status.
This is just one way a nurse can identify a problem simply by implementing a daily practice, which increases the quality of patient care and deliver the most cost-effective nursing care possible.
Dr. Wagner encourages nurses to check online resources that recommend nursing interventions for preventing common types of HAIs. The CDC’s latest recommendations are compiled in the 2009 Guideline for Prevention of CAUTIs and in the Guideline for Prevention of Surgical Site Infection, 1999.
Nurses interested in planning, implementing and evaluating infection prevention and control measures should consider making this their career specialty. Earning a degree in this growing field, such as an MSN with an infection prevention and control specialization, is one way to ensure knowledge of best practices – and perhaps new career opportunities.
For more information or to register for American Sentinel University’s MSN, infection prevention and control specialization, visit http://www.americansentinel.edu/health-care/m-s-nursing/m-s-nursing-infection-prevention-and-control.
For more information or to register for American Sentinel University’s health care and nursing programs, visit http://www.americansentinel.edu/health-care.
About American Sentinel University
American Sentinel University delivers the competitive advantages of accredited online nursing degree programs in nursing, informatics, MBA Health Care, DNP Executive Leadership and DNP Educational Leadership. Its affordable, flexible bachelor’s and master’s nursing degree programs are accredited by the Commission for the Collegiate Nursing Education (CCNE). The university is accredited by the Distance Education and Training Council (DETC). The Accrediting Commission of DETC is listed by the U.S. Department of Education as a nationally recognized accrediting agency and is a recognized member of the Council for Higher Education Accreditation.


 When you think of a nurse, what’s the first image that comes to mind? Chances are, you think of a woman — and for good reason. The vast majority of professional nurses in the U.S. are white women. In fact, only about six percent of nurses are male and, Considering males make up approximately half of the population and minorities are 30 percent, there’s a major disparity in the profession.
When you think of a nurse, what’s the first image that comes to mind? Chances are, you think of a woman — and for good reason. The vast majority of professional nurses in the U.S. are white women. In fact, only about six percent of nurses are male and, Considering males make up approximately half of the population and minorities are 30 percent, there’s a major disparity in the profession.

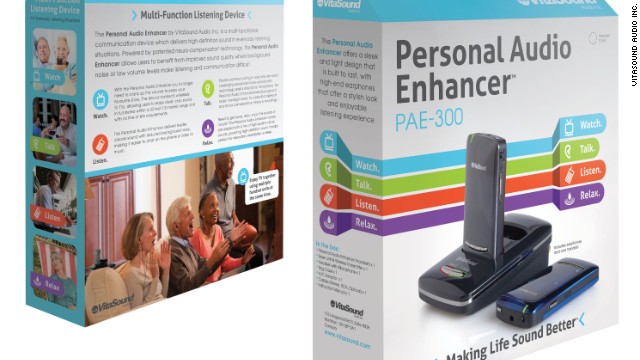
 From "let there be sound" to "let there be light," the next Father's Day gadget is the
From "let there be sound" to "let there be light," the next Father's Day gadget is the 
 The
The  Source:
Source:  As a health care giver, you have a responsibility to ensure that they have adequate knowledge in order to provide competent
As a health care giver, you have a responsibility to ensure that they have adequate knowledge in order to provide competent 


 Source:
Source: