Faced with a shift in the healthcare landscape toward outcomes-based practices and quality improvements, the American Association of Colleges of Nursing (AACN) sought to update the scope of nursing practice with a new master's prepared role: the clinical nurse leader (CNL).
The first new nursing role in over 35 years, the CNL grew out of the 1999 Institute of Medicine report "To Err is Human" which challenged care providers to reduce medical errors and focus on patient safety.
Rising to the challenge, the AACN initiated an investigation into the barriers to improved care delivery and in 2005 introduced the new role as a way to prepare nurses to thrive in the changing healthcare system, according to the AACN website. For many, it couldn't have come at a better moment.
"We are at a pivotal time for the role," said Bob LaPointe, MS, MSN, RN, CNL, president, Clinical Nurse Leader Association (CNLA), and MICU staff nurse at Penn Presbyterian Medical Center, Philadelphia.
"Healthcare is increasingly complex, and we need leaders who are trained in complexity theory to be able to navigate that and understand it to have better patient outcomes and that's what clinical nurse leaders are uniquely trained to do."
CNL
As defined by the CNLA, the CNL is an advanced clinician who serves at the point of care as the lateral integrator, facilitating, coordinating and overseeing care within the unit while also collaborating across the healthcare continuum.1 The CNL is trained to facilitate evidence based care at the bedside and ensure positive outcomes for even the most complex patients. Such training, especially these days, is a great option for nurses of all kinds looking for a way to make a difference at the bedside.
"The role really is about improving clinical outcomes-improving the care of the patient as well as improving financial outcomes," said Tracy Lofty, MSA, CAE, director, Commission on Nurse Certification (CNC), an autonomous agency of AACN, Washington, DC. "Regardless of practice setting, the ultimate goal is to improve outcomes, so really everyone benefits from the role."
When Veronica Rankin, MSN, CNL, Carolinas Medical Center, Charlotte, N.C., decided to go back to school, she chose to do so through a CNL program after her facility's assistant vice president introduced the role at a town hall meeting. Since graduating in 2011, she and her fellow CNLs have been making a huge difference for patients, colleagues and the hospital as a whole.
"We bring that continuity of care back to the bedside, so that even though the nurses may change every shift every day, you are still going to have the same clinical nurse leader Monday through Friday taking care of that patient," Rankin said.
"It has given me the opportunity to stand back and see the big picture of my patients' journey. I can get in there and see, 'OK, out of everyone that is involved in this patient's care, we have all these hands in this pot, what are we missing and where are the bridges I need to help connect?'"
Rankin's ability to streamline care and improve both patient and hospital outcomes comes directly from her training, and nurses and facilities across the nation are starting to see the difference CNLs can make on a unit-by-unit basis.
 "When you take a policy and implement it in your unit, in your hospital, in this city, with the resources you have available, it can be the best evidence based practice out there," LaPointe emphasized. "But we have to apply it to our patients and our staff as well, and that's really where the clinical nurse leader's role really comes into play. How does this make sense for us as a unit, and for our patients."
"When you take a policy and implement it in your unit, in your hospital, in this city, with the resources you have available, it can be the best evidence based practice out there," LaPointe emphasized. "But we have to apply it to our patients and our staff as well, and that's really where the clinical nurse leader's role really comes into play. How does this make sense for us as a unit, and for our patients."
Education
Since the pilot program that tested in the fall of 2006, more than 2,500 nurses have earned CNL certification from CNC. Part of the success, according to LaPointe, is the fact that anyone inspired to become a CNL can do so.
"Nursing has always had multiple points of entry, which leads to lots of people being able to do it, but it also leads to lots of variability about the training and preparation," LaPointe said. "There is so much more to know and healthcare is so much more complex, that to have training in complexity theory, change management and in the science of outcomes, that's going to be good for anybody."
To make the CNL educational track available to nurses already practicing as well as those looking to get into the field, the AACN created five different models so that regardless of educational background, there is an entry into a CNL education program. The five models are:
- Model A - Master's degree program designed for BSN graduates
- Model B - Master's degree program for BSN graduates that includes a post-BSN residency that awards master's credit
- Model C - Master's degree program designed for individuals with a baccalaureate degree in another discipline
- Model D - Master's degree program designed for ADN graduates (RN-MSN)
- Model E - Post-master's certificate program designed for individuals with a master's degree in nursing in another area of study2
Following graduation of a CNL education program, licensure as a registered nurse, and successful completion of the CNL Certification Exam, candidates may be awarded the CNL credential.
With the role gaining momentum, the CNC decided to revamp the certification exam in 2012 to make sure it reflected the basic competencies of a CNL.
"The new exam is based on a CNL job analysis study that was completed in 2011, so the exam reflects the knowledge, skills and abilities of a competent CNL," Lofty said. "It's all about application, so you may be in an educational program, but then you need to be able to apply the knowledge, and that is demonstrated on the exam."
Integration
As new CNL graduates start the search for the right clinical setting, they need to keep in mind that some healthcare organizations have yet to fully integrated the clinical nurse leader into their staffing model.
"There are many healthcare institutions specifically recruiting to full clinical nurse leader positions," said Lofty. "For other institutions, it may not be that title, there may be a different title like care coordinator, or they are still looking for someone with the same skill set and they are still hiring individuals with those competencies and perhaps applying them to other positions."
But CNLs need not worry about their job prospects, because their CNL skills are valuable in just about every care setting. According to a 2012 survey conducted by the CNC, 96% of the respondents indicated that they apply their CNL knowledge in their current role, 92% feel they are an important member of their team and 87% said they are valued as an employee because they are a CNL.3 LaPointe knows from personal experience just how useful being a CNL can be regardless of job title.
"I am not functioning in a job that is called 'CNL' right now, and that is true for many people who currently have the certification," LaPointe said, who was confident he would still use his training despite not being hired specifically as a CNL. "I helped write our successful Beacon Gold application, I was very involved in our hospital's first Magnet designation, I am on the evidence based practice committee for the hospital, and the chair of our unit-based council as part of the shared governance structure of the MICU, so I am using this stuff all the time."
Next Steps
No matter where CNLs end up, they are sure to improve care coordination, communication and hospital-wide outcomes.
"You are basically in there improving care for nurses, patients, and physicians," Rankin said. "You are improving care delivery and the receiving of care for the patient population, so you are in there with your hands so much."
"Bring evidence based practice to your unit to show what the worth of the role is," Rankin advised nurses considering the CNL role. "In the end we are also taught that the clinical nurse leader is the guardian of the nursing profession, so we have to get in there and be the guardian. I would say, go for it, go hard, and be a guardian for the nursing profession."
Source: Advance for Nurses




 "When you take a policy and implement it in your unit, in your hospital, in this city, with the resources you have available, it can be the best evidence based practice out there," LaPointe emphasized. "But we have to apply it to our patients and our staff as well, and that's really where the clinical nurse leader's role really comes into play. How does this make sense for us as a unit, and for our patients."
"When you take a policy and implement it in your unit, in your hospital, in this city, with the resources you have available, it can be the best evidence based practice out there," LaPointe emphasized. "But we have to apply it to our patients and our staff as well, and that's really where the clinical nurse leader's role really comes into play. How does this make sense for us as a unit, and for our patients."

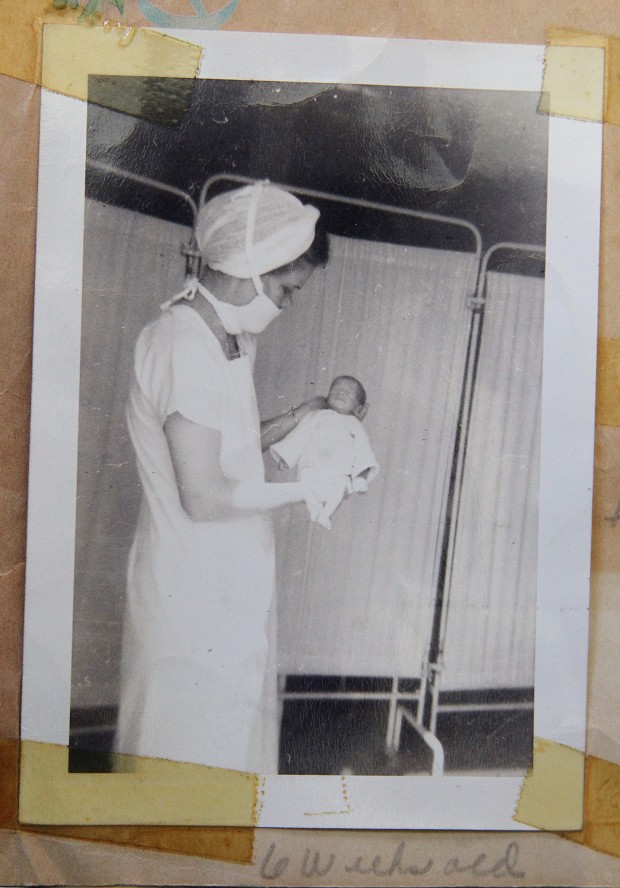 there — remembers feeding Bolles a teaspoon of breast milk from a medicine dropper every hour.
there — remembers feeding Bolles a teaspoon of breast milk from a medicine dropper every hour.








