 I think most Nurses would agree with the statement, "I don’t think I could not help someone." In your private life, I’m sure you’ve been in more than one situation where you jumped in to help someone in need without even thinking of a potential negative impact on you. You’re trained to help people.
I think most Nurses would agree with the statement, "I don’t think I could not help someone." In your private life, I’m sure you’ve been in more than one situation where you jumped in to help someone in need without even thinking of a potential negative impact on you. You’re trained to help people.Decades ago, Ann Rhodes and her husband were coming home from a movie on New Year’s Eve. A car passed them and spun out of control into a field. One person was thrown from the vehicle, which then tragically rolled onto him.
“We stopped and got out of the car. One man was still in the vehicle, but he survived because he had his seat belt on. He had minor injuries,” Rhodes says.
When she got to the other man, he was still alive. Rhodes, an RN with a master’s degree in nursing, took off her coat to put over him and held his hand. Moments later, he died.
“It was pretty awful, and we haven’t gone out on that holiday since. But I believe it is in most people’s instinct, especially a mother’s instinct, to protect others. I don’t think I could not help someone. Most people would stop – nurse or not – to see if they could help someone,” she says.
A Nurse’s Dilemma
Unfortunately, it’s not always as simple as just trying to help. The dilemma of whether or not to get involved while off-duty can be quite a difficult situation for nurses and other healthcare professionals to find themselves in.
Though the accident she witnessed affected her deeply, Rhodes also understands why a nurse might not stop to help. After attempting to render aid, some nurses have actually been the subject of legal action.
“Being sued changes the way you think and the way you practice your profession,” she says.
When The Law Is Not Enough
Every state has some form of the Good Samaritan law, which is designed to protect citizens from being sued or charged criminally for any injuries or death after they’ve stopped to help. The law is meant to encourage bystanders to render emergency assistance by covering everyone, no matter what their profession. However, the law doesn’t provide a rescuer complete immunity.
In a clinic or hospital setting, nurses are often protected through professional liability or Error and Omissions insurance. Rhodes discusses some of the aspects of that protection.
“There will be some exceptions, like if the nurse does something that is illegal or a violation of the law. Lots of policies have exclusions that include things like risky and unclear behavior, or an assault against a patient,” she says. “If they do perform a procedure, like grab a scalpel, and do something they are not trained to do, then that’s a different story.”
Similarly, the Good Samaritan law also does not cover you if you do something reckless. An example of recklessness would be starting to render aid, then stopping and leaving before the patient has been stabilized or other help has arrived.
However, if you give a good faith effort given the circumstances, you have probably met your legal requirements and will likely be covered by the law. However, that doesn’t mean you won’t get sued.
“People can file a lawsuit against anyone. The issue is whether they can collect,” Rhodes says.
“Even if the lawsuit isn’t successful, it still takes an emotional toll on the person being sued. It will be costly too, even if the person being sued did everything right. They have to defend themselves.”
Enabling Bystander Response
The American Nurses Association (ANA) states on its website that registered nurses have consistently been reliable responders even when it puts their own safety or well-being at risk.
Yet others struggle with the call to respond for a variety of reasons.
These may include not having adequate support to meet the needs of the patient, concern about professional ethics, or legal protection while providing care.
Fortunately, the ANA and other national associations are partnering with government groups, employers, and others to help. By implementing policies that enable registered nurses and others who provide care to respond without fear, it helps to ensure that the needs of the American public are met during any kind of disaster.
Assessing An Emergency Situation
So what should you do if you find yourself in an emergency situation?
Carolyn Buppert, a healthcare attorney and author of the book “Nurse Practitioner’s Guide to Compensation and Qualify: How to Get Paid and Not Get Sued,” offers some sage advice.
“Nurses are not obligated to help,” she says. “In an emergency situation, it’s tough to think of precautions or liability. But what should a nurse think about when she comes upon an individual or group of people who need medical attention outside of the workplace?”
Buppert recommends several questions to ask before rendering aid:
- What does this person need?
- How much of an emergency is this?
- What do I have to offer?
- Is anyone already helping?
- Am I sufficiently educated and experienced to provide a useful service to this person?
- What is the potential for physical danger to myself?
- What are the chances that EMS will be here soon?
- What is the likelihood that EMS will get here in time?
“The law can get tricky in situations. For instance, if a nurse works for a hospital, and a discharged patient calls the nurse or approaches her or him in a shopping mall asking questions or requesting services or advice, the nurse should decline to provide nursing services or advice, and tell the patient to contact their physician’s office,” Buppert says.
“If the nurse gives advice and the advice is wrong, the patient suffers some adverse outcome, the nurse could be sued, and there is no Good Samaritan law that would protect the nurse,” she adds.
Preparing Before An Emergency
Not every form of ‘helping’ is covered by Good Samaritan laws. Some states’ laws cover motor vehicle accidents but not all incidents or stranger’s needs on the street.
Buppert gives one last suggestion for all nurses. “My advice to nurses is to look up the Good Samaritan law in your state and see what protection it offers. Many nurses will help others, while off duty, without thinking of the possible consequences to themselves,” she says. “That’s admirable, but it doesn’t hurt to spend a few minutes looking at your state’s law to see what protections are available at a time when there is no emergency.”
Have a question about this or any general questions? Ask one of our Nurse Leaders!




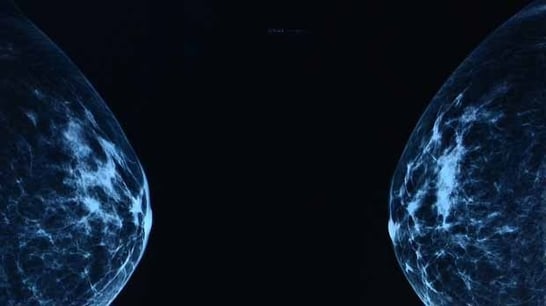 Mammograms, we know how barbaric and uncomfortable the procedure is for all of us. I often find myself thinking, there’s got to be a better way. Wouldn’t it be great if we had something that gives a better picture, doesn’t use radiation, and doesn’t flatten our breasts during the process? We’d all like to skip our mammograms entirely, but the prospect of early cancer detection keeps us going back year after year.
Mammograms, we know how barbaric and uncomfortable the procedure is for all of us. I often find myself thinking, there’s got to be a better way. Wouldn’t it be great if we had something that gives a better picture, doesn’t use radiation, and doesn’t flatten our breasts during the process? We’d all like to skip our mammograms entirely, but the prospect of early cancer detection keeps us going back year after year.

 The holiday season is fast approaching and with that comes a lot of stress in both our personal and professional lives. No matter what holiday you celebrate, we hope it is a joyful and peaceful holiday for you and your family.
The holiday season is fast approaching and with that comes a lot of stress in both our personal and professional lives. No matter what holiday you celebrate, we hope it is a joyful and peaceful holiday for you and your family. If you’re thinking about continuing your education or are just starting out with your Nursing education, we think this article might be helpful to you. Let us know what you think.
If you’re thinking about continuing your education or are just starting out with your Nursing education, we think this article might be helpful to you. Let us know what you think. This is an article that might be right up your alley. It’s about things people say to Nurses. Sometimes comments are made that are totally innocent and mean no harm. Other comments are just plain ignorant, annoying, insulting, stupid or rude and usually the commenter has no idea they are being offensive.
This is an article that might be right up your alley. It’s about things people say to Nurses. Sometimes comments are made that are totally innocent and mean no harm. Other comments are just plain ignorant, annoying, insulting, stupid or rude and usually the commenter has no idea they are being offensive. When working closely with patients that are undergoing tests or admitted to the hospital for several days, do you find they look to you for their emotional and spiritual needs as well as their physical needs? If your answer is yes, how do you help them with their spiritual needs? Do you feel this is something beyond your training and scope of experience? Do you see it as a necessary part of your job? Are you comfortable with it?
When working closely with patients that are undergoing tests or admitted to the hospital for several days, do you find they look to you for their emotional and spiritual needs as well as their physical needs? If your answer is yes, how do you help them with their spiritual needs? Do you feel this is something beyond your training and scope of experience? Do you see it as a necessary part of your job? Are you comfortable with it?
 Technology continues to make strides in both our professional and personal lives. This article is about a robot that’s being tested to deliver medication to chemo patients, thus eliminating the step of having to wait in line for medication after a very lengthy day of chemo. This is a new technology being tested at Dana Farber Cancer Institute and patients are enthusiastic about it.
Technology continues to make strides in both our professional and personal lives. This article is about a robot that’s being tested to deliver medication to chemo patients, thus eliminating the step of having to wait in line for medication after a very lengthy day of chemo. This is a new technology being tested at Dana Farber Cancer Institute and patients are enthusiastic about it. We here at DiversityNursing.com have the greatest respect and appreciation for what Nurses do in their profession every day. We value your education, experience, compassion, kindness, great advice and appreciate you being there when your patients need you. The healthcare system couldn’t exist without Nurses. You make the hospitals, clinics, out-patient centers, schools and insurance companies be able to do what they are in business to do. In short… you are amazing!
We here at DiversityNursing.com have the greatest respect and appreciation for what Nurses do in their profession every day. We value your education, experience, compassion, kindness, great advice and appreciate you being there when your patients need you. The healthcare system couldn’t exist without Nurses. You make the hospitals, clinics, out-patient centers, schools and insurance companies be able to do what they are in business to do. In short… you are amazing! It’s fascinating how people’s minds work. Some people take something that is very complicated to most, and break it down in very simple terms so it’s easy to understand. And some people see a problem and figure out a way to fix it or make what currently exists better. Right now, we’re hearing about Nobel prize winners who have done something amazing in their field. There are also young people doing very interesting things to help their fellow man as well.
It’s fascinating how people’s minds work. Some people take something that is very complicated to most, and break it down in very simple terms so it’s easy to understand. And some people see a problem and figure out a way to fix it or make what currently exists better. Right now, we’re hearing about Nobel prize winners who have done something amazing in their field. There are also young people doing very interesting things to help their fellow man as well.