 At the beginning of your Nursing career, you have many decisions to make. One of the biggest is what shift works for you. When you’re first starting out, you may not have a choice. You have to take what is available. However, if you do have a choice, this information provides what each shift has to offer.
At the beginning of your Nursing career, you have many decisions to make. One of the biggest is what shift works for you. When you’re first starting out, you may not have a choice. You have to take what is available. However, if you do have a choice, this information provides what each shift has to offer.
Day Shift
More activity
Day shift Nursing is more active. Patients are awake, phones are ringing, more call lights are going off and families are visiting patients. If you enjoy the fast paced environment then you should consider working the day shift.
More staff present
According to an article by Nurse Blake, there is help and different opportunities for learning during day shift because more people work during the day. Have an urgent question for the physician, dietitian, wound care specialist, or physical therapist? No worries, most departments have staff available during the day to help assist with any questions. Also, numerous procedures/tests take place during the day which can provide opportunities to observe and learn new skills.
Fits in with regular daily schedules
It's easier to maintain a social life because you'll be able to attend more nightly or weekend activities with family and friends. You'll also be able to keep an ordinary sleep schedule.
Cafeteria is open
Sometimes the cafeteria isn't open 24/7. So during the day shift you don't have to worry about forgetting a lunch! You can grab a snack whenever if you become hungry.
Team bonding
It's nice to go out with your coworkers after a long shift and grab dinner or drinks to unwind, have a few laughs and get to know each other outside of the work environment. If you work night shift, you have less opportunities to go out somewhere besides a breakfast place.
Night Shift
More money
An article by Nursingjobs.com said, many hospitals offer shift differentials at hourly rates to help supplement a Nurse's income in return for working night shifts.
According to PayScale, the average hourly rate for an RN working the day shift is between $22.54 - $40.69/hour, depending on geographical location, experience level, and medical facility. A night Nurse, on the other hand, can expect to make up to $41.03/hour, which is slightly higher. The added night shift differential varies by facility type, but it can make a big difference over long-term periods.
Less traffic and better parking
You can get your errands done during the day while most people are at work. Your drive to work should be shorter because there are less people on the road at night. A shorter commute means more sleep! There will be less people parked at your job so that means better parking.
Quieter
Usually during the night shift, patient volumes are generally lower. It can be busy during the first few hours of the shift but as the night goes on it settles down. So you'll have fewer distractions, less discharges to process, and fewer medications to administer. Also, you'll have more time to spend with each patient as there are limited visitors and family members present.
2 or 3 Days a Week
A Shorter Work Week
According to an article from Nurse.org, usually working three days a week means having four days off. This is a great option for Nurses with a long commute because it translates into less hours on the road. Also, those requiring child care prefer this option instead of the traditional 8-hour schedule.
Reducing Errors and Providing Better Care
Rather than having three Nurses in a 24-hour period, a patient will have two, a day Nurse and a night Nurse. Since only two Nurses are transferring information, there is less risk for miscommunication errors. The Joint Commission reported that at least 80% of serious medical errors result from a miscommunication between caregivers during handoff.
Flexible Schedule
Most Nurses working 12-hour shifts group their work days together and have longer periods of time off. This leaves time for traveling, a side job, education, or time with family and friends.
What is your current schedule? Have you worked different shifts? If so, which do you prefer and why? We would love to hear what you think! Please comment below!



 According to a
According to a  Smart phones help Nurses stay on top of their game. You can download apps that help you study for an exam or find out information about a specific drug. Mobile apps have provided a variety of tools for Nurses. Below you will find some of the top mobile apps for Nurses.
Smart phones help Nurses stay on top of their game. You can download apps that help you study for an exam or find out information about a specific drug. Mobile apps have provided a variety of tools for Nurses. Below you will find some of the top mobile apps for Nurses. 
 You may want to consider a career as a Nurse Educator if you're interested in teaching or passionate about medical research and public policies.
You may want to consider a career as a Nurse Educator if you're interested in teaching or passionate about medical research and public policies.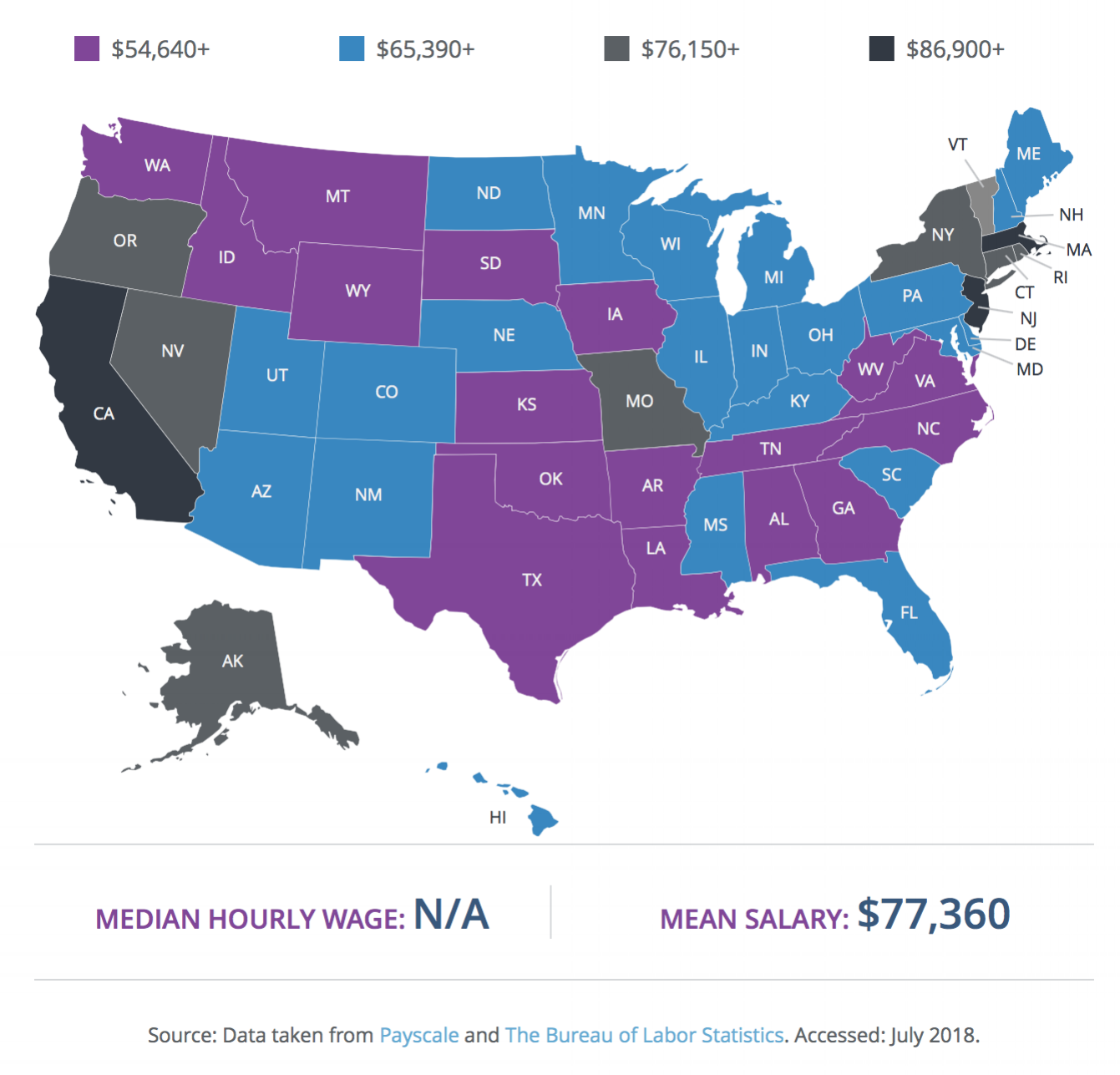
 Palliative care, end-of-life care, and hospice care share a common goal: to relieve suffering. But there are also important distinctions.
Palliative care, end-of-life care, and hospice care share a common goal: to relieve suffering. But there are also important distinctions. NPR
NPR RALEIGH – The North Carolina Nurses Association (NCNA) and its charitable arm, the North Carolina Foundation for Nursing (NCFN) are announcing an emergency campaign to provide support to nurses who have suffered loss or damages from Hurricane Florence. The NCFN - Nurse Recovery Fund seeks tax-deductible donations whose sole purpose is to help nurses get back on their feet sooner; NCNA and NCFN believe that helping nurses return to their normal lives will benefit the entire state.
RALEIGH – The North Carolina Nurses Association (NCNA) and its charitable arm, the North Carolina Foundation for Nursing (NCFN) are announcing an emergency campaign to provide support to nurses who have suffered loss or damages from Hurricane Florence. The NCFN - Nurse Recovery Fund seeks tax-deductible donations whose sole purpose is to help nurses get back on their feet sooner; NCNA and NCFN believe that helping nurses return to their normal lives will benefit the entire state. Forensic Nurses provide healthcare to those incarcerated in the criminal justice system in a variety of settings such as jails, prisons, and juvenile detention centers.
Forensic Nurses provide healthcare to those incarcerated in the criminal justice system in a variety of settings such as jails, prisons, and juvenile detention centers.  An active shooter incident is something no nurse wishes to experience. Unfortunately, these situations can, and do, happen at healthcare organizations across the country.
An active shooter incident is something no nurse wishes to experience. Unfortunately, these situations can, and do, happen at healthcare organizations across the country.