Underserved communities often face significant barriers to accessing equitable healthcare. To make meaningful progress, these communities need to see themselves reflected in the systems designed to improve their health. This requires a commitment to Diversity and Inclusion across all aspects of healthcare.
The Role of Representation in Healthcare
Healthcare systems must prioritize the lived experiences, preferences, and concerns of individuals, considering factors such as gender, geography, and cultural background. Evidence shows diverse voices lead to more effective solutions and better health outcomes. By including a broader range of perspectives, we can identify blind spots and address unmet needs with sensitivity and precision.
This change must extend across industries, from pharmaceutical companies creating life-saving medicines to hospitals staffed by Doctors and Nurses who understand the unique challenges of the populations they serve. Universities shaping the next generation of medical professionals must also prioritize diversity to ensure future providers are equipped to connect with and care for diverse communities.
However, it’s not just about inclusion, it’s also about rebuilding trust. Many underserved communities have experienced a long history of neglect or bias in healthcare, leading to deep-rooted mistrust. Improving representation and fostering inclusivity is key to restoring confidence and ensuring better health outcomes for all.
Persistent Health Inequities
Despite advancements in healthcare, inequities persist:
- Women are more likely to die after a heart attack than men.
- Black women have a higher likelihood of dying from breast cancer compared to white women.
- Rural communities consistently experience poorer health outcomes than urban areas.
Health disparities are directly related to the unequal distribution of social, political, economic, and environmental resources, which manifests in various ways across different communities.
Socially, marginalized groups often lack access to quality education and employment opportunities, which can lead to lower income levels and limited access to healthcare services.
Politically, these communities may have less representation and influence in decision-making processes, resulting in policies that do not adequately address their specific health needs.
Economically, the gap in wealth distribution can mean underserved populations struggle to afford necessary medical care, nutritious food, and safe housing.
Environmentally, these communities might reside in areas with higher pollution levels or limited access to clean water and green spaces, further exacerbating health issues.
Addressing these disparities requires a comprehensive approach that considers all these interconnected factors to create a more equitable healthcare system for all.
Workforce Inclusivity: A Path to Health Equity
Creating an inclusive healthcare workforce is critical for driving innovation and addressing inequities. Diverse teams foster creativity, uncover blind spots, and develop transformative solutions that meet the needs of underserved populations. This approach encourages the development of medicines and treatments that reflect the lived experiences of diverse communities.
Inclusion also strengthens relationships between healthcare providers and patients. When patients feel heard and represented, trust improves, leading to better communication, more accurate diagnoses, and more personalized treatments.
Programs Driving Change
Globally, organizations are taking steps to improve diversity and representation in healthcare. For example:
- The World Health Organization’s Global Knowledge Network for Health Equity (GKNHE) aims to address social determinants of health.
- The American Medical Women's Association's Gender Equity Task Force aims to achieve gender equity in society, starting with the healthcare industry, through education, action, and collaborations.
- The Novartis US Foundation’s Beacon of Hope initiative works with historically Black colleges and universities (HBCUs) to tackle health disparities. This program aims to increase clinical trial participation, support research into health inequities, and develop future healthcare leaders.
A Call to Action
The journey to health equity requires collective effort and sustained focus. Prioritizing Diversity and Inclusion is not just the right thing to do, it’s essential for improving outcomes and rebuilding trust with underserved communities. As we face the health challenges of the future, let’s ensure inclusivity remains at the forefront of healthcare innovation, education, and delivery.
By working together, we can create a healthcare system that truly serves everyone.


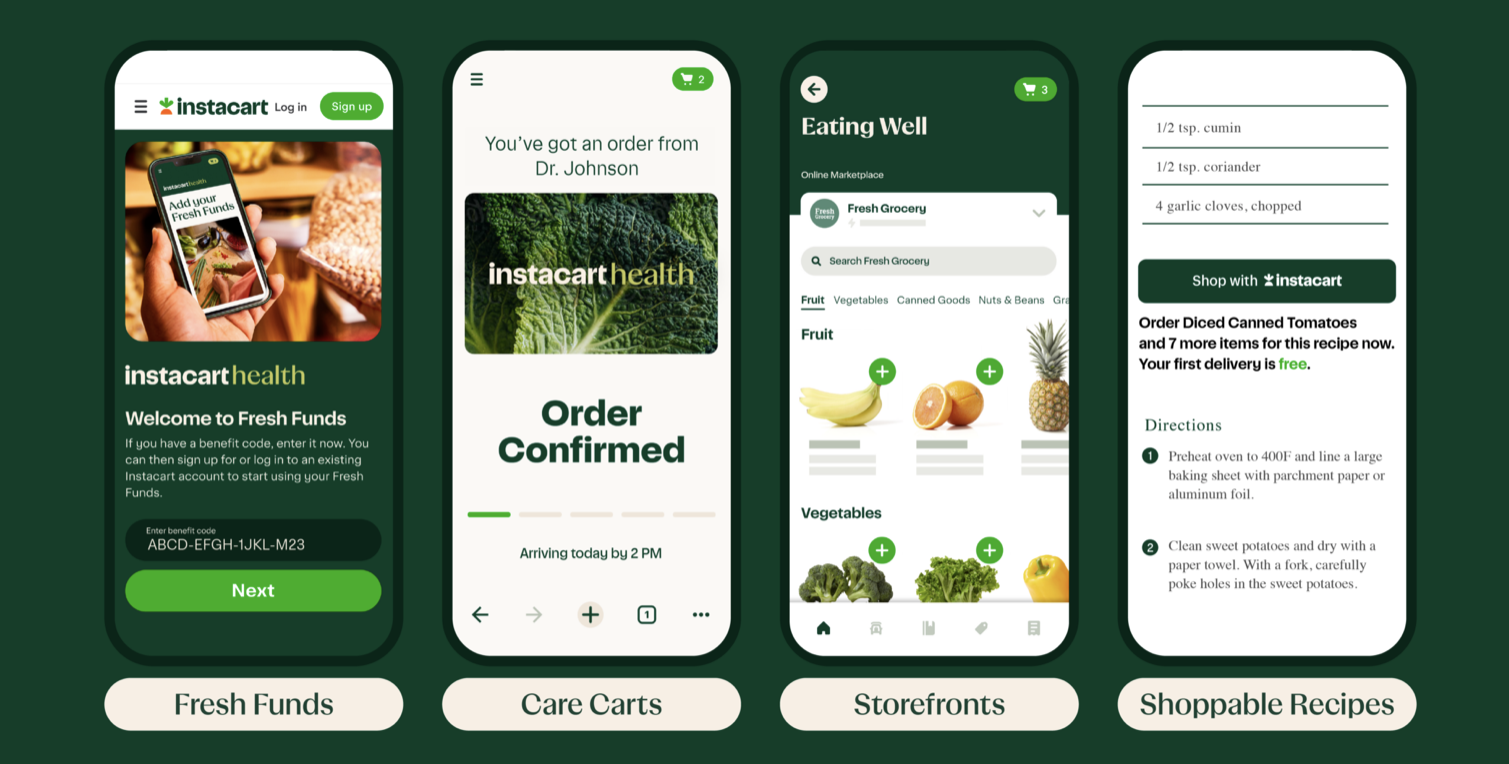 Healthcare providers recognize the crucial role nutritious diets play in promoting and maintaining good health. People with healthy eating patterns
Healthcare providers recognize the crucial role nutritious diets play in promoting and maintaining good health. People with healthy eating patterns  Last year, Chief Diversity Officer (CDO) hires grew by 84%, making it the fastest growing C-suite title, according to
Last year, Chief Diversity Officer (CDO) hires grew by 84%, making it the fastest growing C-suite title, according to 

 Women of color in the United States suffer unacceptably poor maternal health outcomes, including high rates of death related to pregnancy or childbirth.
Women of color in the United States suffer unacceptably poor maternal health outcomes, including high rates of death related to pregnancy or childbirth. The policy released by
The policy released by  Research has documented a number of
Research has documented a number of 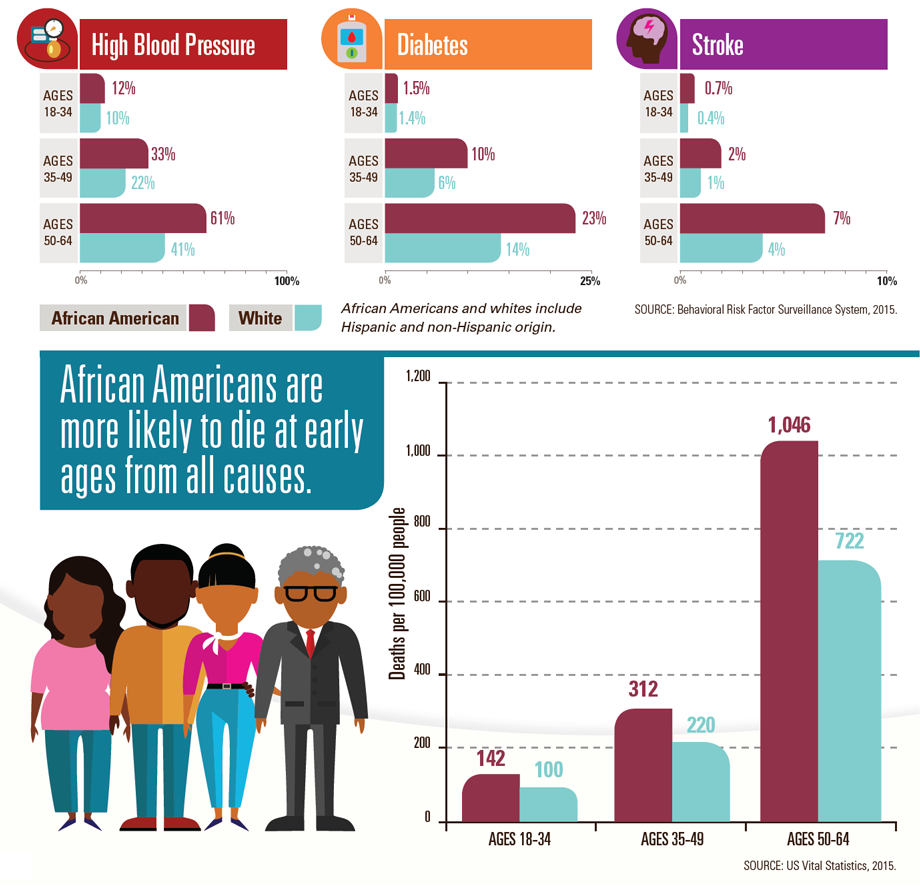



 Frontier Nursing University conference discusses healthcare diversity
Frontier Nursing University conference discusses healthcare diversity