 An estimated 4%, or about 150,000, Nurses in the U.S. are Filipino, but comprise nearly a third of Registered Nurse deaths due to COVID-19.
An estimated 4%, or about 150,000, Nurses in the U.S. are Filipino, but comprise nearly a third of Registered Nurse deaths due to COVID-19.
Business Insider reported, Nurses of Filipino descent account for 31.5% of the workforce's COVID-19 deaths.
In California, where about 20% of Nurses identify as Filipino, they account for nearly 70% of COVID-19 deaths in the profession, according to the Mercury News. Statewide, Asian Americans make up about 5% of coronavirus cases and 11.7% of deaths, compared to their 15% of the population.
Zenei Cortez, an RN who works at Kaiser Permanente’s South San Francisco Medical Center and, as co-president of the California Nurses Association/National Nurses United worries that her fellow Filipino Nurses are less likely than other Nurses to demand workplace protections.
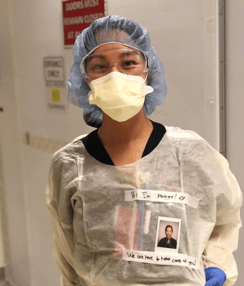
“Culturally, we don’t complain. We do not question authority,” Cortez said. Many Filipino Nurses feel a strong sense of group loyalty, or the importance of putting the welfare of the group over that of the individual; in Tagalog, the word is pakikisama. “We are so passionate about our profession and what we do, sometimes to the point of forgetting about our own welfare,” she said. “We treat our patients like they are our own family.”
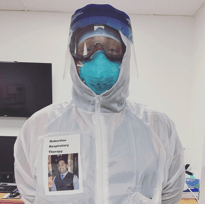
It’s the lack of proper PPE that has pushed some Filipino Nurses to speak out, when in the past they stayed silent about their working conditions.
“What I am seeing now is that my colleagues who are of Filipino descent are starting to speak out,” Zenei said. “We love our jobs, but we love our families too.”
Catherine Ceniza Choy, a professor of ethnic studies at UC Berkeley whose work has focused on the history of Filipino American Nurses said, Filipino American Nurses are more likely to work in higher risk roles such as the intensive-care unit, emergency medicine or telemetry, putting them directly in the path of COVID-19.
“Filipino Nurses, here specifically in the U.S., are concentrated specifically in in-patient critical care services,” Choy said. “Many of them are also caregivers at home, not only of children, but also their parents and other elders. And so part of the problem with the pandemic is these multiple layers of vulnerability and exposure.”
Jollene Levid and other volunteers have been keeping track of Filipino health care workers who've died from the disease worldwide. Their website, Kanlungan.net, which means shelter or refuge, is an online memorial with pictures and stories of those who've been lost.
The website reads "KANLUNGAN is intended to be a memorial to the transnational people of Philippine ancestry who make up a huge sector of the global healthcare system. This is to remember them as human beings, not simply as a labor percentage, a disease statistic, or an immigration number. And since the Internet is forever, we hope that KANLUNGAN will keep reminding the world of the skills, dedication, and the self-sacrifice demanded of health care workers so humanity may be healed."







 Bonnie Castillo, is the Executive Director of National Nurses United (NNU) and a former Intensive Care Nurse.
Bonnie Castillo, is the Executive Director of National Nurses United (NNU) and a former Intensive Care Nurse. 
 What Nurses Need to Know about COVID-19
What Nurses Need to Know about COVID-19