 1. Nursing Central
1. Nursing Central
Unbound Medicine’s award-winning Nursing Central app is available on Android and iOS devices. Users are satisfied with its extensive drug and disease information. Nurses and students are able to work more efficiently thanks to Nursing Central providing detailed information on diseases, tests, drugs and procedures on the go.
What users are saying:
“This app is awesome! I love that it has all the necessary references. The search is great and pulls up the item in all the references…”
Rating: 
Cost: Free
Available: Android and iTunes
 2. Diseases Dictionary
2. Diseases Dictionary
A free Android and iOS app, Diseases Dictionary offers a long list of illnesses and conditions nurses are apt to encounter, along with symptoms and preferred treatments. Nurses and students can type in the symptom and a list of possible diseases will appear; this app provides comprehensive information about how to deal with symptoms/how to prevent the disease; and how to improve knowledge about diseases.
What users are saying:
“High informative. I recommend this app.” “A Must-Have app! What an educative app!”
Rating: 
Cost: Free
Available: Google Play and iTunes
 3. Black’s Medical Dictionary
3. Black’s Medical Dictionary
For over a century, medical professionals have relied on Black’s Medical Dictionary. With over 5,000 definitions of medical terms, this app features a navigational display with rich media experience; user-friendly, intuitive interaction; and the ability to share with friends using social media features. Reviews are mixed, with some users complaining of the app’s $14.99 price tag.
Rating: 
Cost: $14.99
Available: Google Play and iTunes
 4. The Color Atlas of Family Medicine
4. The Color Atlas of Family Medicine
2,000 full-color photographs will help you visually diagnose common and uncommon conditions and diseases encountered in clinical practice. At $124.99, it’s not ideal for nurses on a budget — but satisfied users report that the app’s thorough explanations and color pictures are well worth the money.
What users are saying:
“Full of pictures and useful facts about diseases and treatments…I refer to it often in my practice.” “Great primarily outpatient reference.” “Very impressed with the app, good photo resolution when searching for specifics.”
Rating: 
Cost: $124.99
Available: Google Play and iTunes
 5. Merck Manual
5. Merck Manual
The oldest continuously published textbook for English-speaking medical professionals, the Merck Manual is free on iTunes. This app includes “How to Do” videos on numerous outpatient procedures and physical examinations; quizzes that check knowledge of medical disorders, symptoms and treatments; interactive case simulations that test the ability to treat a specific patient over the disease course; and editorials written by top medical experts. Some users believe it is a must-have for nurses, but others feel it’s difficult to navigate.
What users are saying:
“I downloaded this new Merck Manuals reference when I saw it first available, and have the home user version too.” “Offline use and excellent interface!”
Rating: 
Cost: Free
Available: Google Play and iTunes
 6. MedPage Today
6. MedPage Today
Get up to date with the latest developments in the medical world with MedPage Today, MedPage is the leading source for breaking medical news, daily coverage of over 30 specialties, annual coverage of over 60 meetings and symposia and free CME and continuing education credits.
What users are saying:
“Very good app for doctors. Awesome and authentic information with reference.” “Best app for medical students, but needs more details.”
Rating: 
Cost: Free
Available: Google Play and iTunes
 7. Pedi STAT
7. Pedi STAT
Satisfied users on iTunes claim that Pedi STAT is the easiest medical app to use. Described as a rapid reference for RNs, paramedics, physicians and other healthcare professionals caring for pediatric patients in the emergency or critical care environment. The Google Play version costs $7.87.
What users are saying:
“Great resource for paramedic, CCP, or ER RN, use it frequently. “Awesome…use this app in clinical situations a lot.”
Rating: 
Cost: $2.99
Available: Google Play and iTunes
 8. NurseTabs: Fundamentals
8. NurseTabs: Fundamentals
The NurseTabs series offers a thorough overview of several important topics, with many concepts discussed in video form. App users will have access to over 120 skills and procedures separated by topic areas learned through fundamental nursing courses. After selecting a skill, you’re presented with the equipment needed to perform the procedure and a step-by-step of how to perform it safely. The app is $9.99, but in-app videos cost another $4.00 — a fact that does not please some users.
Rating: 
Cost: $9.99
Available: Google Play and iTunes
 9. NurseTabs: MedSurg
9. NurseTabs: MedSurg
Another valuable app in the NurseTabs series, MedSurg focuses on diseases and conditions. This app is suited for novice nurses and nursing students with over 340 common diseases and disorders that are separated by the body system. Once a disease/disorder is selected, nursing processes, managing client care and tons of other useful information is at your fingertips. Like Fundamentals, it costs $9.99. The two apps are available in bundle form for $19.99 on Google Play.
What users are saying:
“Good for students, but basic and vague for nursing…” “I am an LPN a charge nurse and I love this app. So easy to use. Every diagnosis u can think of is on the app…”
Rating: 
Cost: $9.99
Available: Google Play and iTunes
 10. Nurse’s Pocket Guide
10. Nurse’s Pocket Guide
The Nurse’s Pocket Guide is constantly updated with new information on diagnosis and interventions. Each diagnosis listing includes a definition, related factors, defining characteristics, prioritized actions/interventions, NIC/NOC classifications and documentation of guidelines. The free app is available on iTunes and Google Play.
What users are saying:
“It’s a good app if you are willing to pay for (in-app purchases).”
Rating: 
Cost: Free
Available: Google Play and iTunes
 11: Voalte One
11: Voalte One
An HIPAA-compliant app, Voalte One provides exceptional communication for caregivers. It provides alarm and nurse alert notifications, text messaging on easy-to-use app. It also offers VoIP calling. This tool helps streamline communications in tough situations. It’s easy to use and provides a way to gather information immediately.
Rating: 
Cost: Free
Available: Android and iTunes
 12. NursingCenter CEConnection
12. NursingCenter CEConnection
Earning continuing education credits can be a challenge, but NursingCenter CEConnection makes it easy. Thanks to this easily accessible app, you can view CE courses and complete them offline whether you’re at home, on your commute or on your shift. Once you return to a wifi connection, your assignments will automatically sync with your CE Planner account and access your certificate.
Rating: 
Cost: Free
Available: Google Play and iTunes
 13. Heather’s Nursing Cheat Sheets
13. Heather’s Nursing Cheat Sheets
Download Heather’s Nursing Cheat Sheets on your Android device and get ready to access the detailed information you need, when you need it. The app has a temperature conversion chart, a neurological coma scale, and several other helpful cheat sheets. It is important to know that the information in this app is compiled from a variety of sources and you should always know your own facility’s protocols.
What users are saying:
“Amazing app! As a RN working bedside in the critical care setting, this is my quick go to tool…” “Great reference tool!” “Awesome! A student nurse’s dream!”
Rating: 
Cost: $2.99
Available: Google Play
 14. Davis’s Drug Guide For Nurses
14. Davis’s Drug Guide For Nurses
With information on over 5,000 generic and brand name drugs, Davis’ Drug Guide is a great and comprehensive tool. With practical information on trade name and generic drugs, each focuses on safety and patient care, including information on dosing and administration, interactions, side effects and patient teaching. The app has numerous rave reviews on Google Play.
What users are saying:
“I love the website, but the app is frustrating because I cannot search medications…” “Fast, easy access to information without having to lug a book around…”
Rating: 
Cost: Free
Available: Google Play and iTunes
 15. Epocrates Rx
15. Epocrates Rx
Available on iTunes and Google Play, Epocrates Rx boasts high ratings on both platforms, and 1 out of every 2 physicians rely on Epocrates to enable better patient care. The app offers detailed information for a wide range of brand, generic, and over-the-counter medications. A one year Epocrates Plus subscription is available for $174.99.
What users are saying:
“Superb guidance.”
Rating: 
Cost: Free
Available: Google Play and iTunes
 16. I.V. Drug Handbook
16. I.V. Drug Handbook
Published by McGraw-Hill, this useful Android app helps nurses successfully carry out one of the profession’s trickiest tasks. It features several helpful learning tools, including a ‘Favorites,’ ‘Recent’ and ‘Word of the day’ features to help you further enhance your vocabulary from an extensive library. The Google Play version is free, but offers in-app purchases.
What users are saying:
“Very ok.” “Stellar”
Rating: 
Cost: $44.99
Available: Google Play and iTunes
 17. NCLEX Flashcards
17. NCLEX Flashcards
Whether you’re currently in nursing school or could use a refresher, the NCLEX Flashcards app has over 1,600 practice questions, quizzes, mnemonics, and strategies. Bonus: If you purchase the mobile version, you’ll be granted access to the full-featured online version. The Google Play version is free, but offers in-app purchases.
What users are saying:
“Love it buy after 2 questions it stops, please fix!” “Excellent! Very helpful and it makes it easy to remember everything.” “Good app for NCLEX review…it does freeze at times.”
Rating: 
Cost: $3.99
Available: Google Play and iTunes
 18. Nursing Guide App
18. Nursing Guide App
Quantum X. Inc’s Nursing Guide App offers a range of information for nursing students and experienced nurses alike. Equipped with mnemonics, articles and tips and quotes, this app was created to share basic to complex information about the nursing field.
What users are saying:
“Very helpful.” “Excellent. More than expected.” “Does not give full info…”
Rating: 
Cost: Free
Available: Google Play and iTunes
 19. Critical Care ACLS Guide
19. Critical Care ACLS Guide
The Critical Care ACLS Guide is the smartphone age’s response to a classic, twenty-year-old booklet that made it easier for nurses to check doses and interpret EKGs. You can have immediate access to critical information loaded with rich content, detailed illustrations and features including quick navigation, expanded search capability, calculators and custom bookmarks.
What users are saying:
“Effective.” “Well designed to provide fast information.” “Better than expected for immediate needs.”
Rating: 
Cost: $7.99
Available: Google Play and iTunes
 20. NurseGrid
20. NurseGrid
Scheduling can be a hassle for nurses, but with iTunes’ NurseGrid, it doesn’t have to be. Used by over 200,000 nurses, the app allows for schedule management across several work sites. Because of this app’s user-friendly features, it only takes a few seconds to create your shift calendar for the next few months. You also have the opportunity to connect with other NurseGrid users who work in your department.
What users are saying:
“Nice app. I love how easy it is to add my work schedule and that my coworker can see my schedule.” “Sluggish, but a great app on iOS.” “It’s okay. It shows my shifts and is easy to add shifts…”
Rating: 
Cost: Free
Available: Google Play and iTunes
 21. Nursing Procedures
21. Nursing Procedures
Nursing Procedures focuses largely on providing nurses the best resources before they begin a procedure. Ranging from assessments to medication administration to code blue situations. As a bonus, you’ll get a Weekly Funny once a week that gives you a funny video, quote, picture or meme to cheer you up. The iTunes version is free.
What users are saying;
“Great app but please add more procedures to the midwifery aspect…” “Please add the requirements for the various procedures. That I think will help us a lot.” “Great app.” “It’s a great app. Easy to use and understand. Big ups.”
Rating: N/A
Cost: $0.99
Available: Google Play and iTunes
 22. Nurses First
22. Nurses First
The Nurses First app features daily nursing tips, fun facts, nurse quote section, Vines section and a giveaway section. Information is pulled from the top nurse blogs and fan sites; everything you need to know in one mobile app.
What users are saying:
“Perfect app for nurses. This one has it all.” “I keep opening this app, even while I’m at work…it just makes the day go well.” “I am so glad I downloaded the nurses first app. LUV it.”
Rating: 
Cost: Free
Available: Google Play
 23. IV Drip Rate Calculator
23. IV Drip Rate Calculator
Most features of the IV Drip Rate Calculator app are available on modern pumps, but modern pumps aren’t always available. With this app you can add a drug amount in mg, mcg, grams or units to a volume of fluid, select the dose ordered and the ml/house necessary to deliver that dose will display. Several satisfied users claim that the app has made their jobs easier.
What users are saying:
“Good math, would be better if you could scroll the screen to the next couple fields..” “Good for when I need to think faster while multi-tasking.”
Rating: 
Cost: Free
Available: Google Play
 24. IV Infusion Calculator
24. IV Infusion Calculator
This simple and straightforward iOS and Android app work whether you are using gravity or pumps. It will give you your answer in mL/hr, gtts/min and gtts/15 seconds. This app also includes an IV Push calculator and a Fluid Rate calculator. The Pro upgrade to the app costs $0.99.
What users are saying:
“Very useful and covers all types of calculations I use.” “I use this app every week.”
Rating: 
Cost: Free
Available: Google Play and iTunes
 25. Nursing Reference Center
25. Nursing Reference Center
Amp up your nursing skills with Nursing Reference Center. The app provides relevant clinical resources to nurses, directly at point-of-care and offers the best available and most recent clinical evidence from thousands of full-text documents. Note: to use the NRC app, you must obtain an access key.
What users are saying:
“Wonderful resource for nursing staff.”
Rating: 
Cost: Free
Available: Google Play and iTunes
 26. Lippincott Nursing Advisor
26. Lippincott Nursing Advisor
Quick answers for pressing medical questions are available on the iOS Lippincott Nursing Advisor app. Although many facilities offer free use of the app, some users must make in-app purchases. You’ll have access to regularly updated clinical content by a team of nurses and clinical subject matter experts as well as the ability to add your own protocols and notes.
What users are saying:
“Time saver. I bought this app mainly to benefit my Lippincott account was such a huge pain…this however has saved me time and headache and I can get it on my phone as well.”
Rating: 
Cost: Free
Available: Google Play and iTunes
 27. Wellbeing For Nurses
27. Wellbeing For Nurses
Stress and fatigue make it a challenge for nurses to stay healthy. Wellbeing For Nurses Magazine aims to combat this with a useful app. You’ll have access to monthly doses of in-depth articles that focus on the fields of health, happiness, and well-being.
What users are saying;
“Perfect…” and “A good one.”
Rating: 
Cost: Free
Available: Google Play
 28. Intensive Care Medicine
28. Intensive Care Medicine
Stay up to date on the latest research with the Intensive Care Medicine app. Google Play users appreciate the free app’s advanced search and article saving capabilities. This app comes from the Intensive Care Medicine journal that continually publishes review articles, original papers, and education articles written by leading members of the medical community.
What users are saying:
“Very nice, but should allow members to use their individual subscriptions to access.”
Rating: 
Cost: Free
Available: Google Play and iTunes
 29. Organs 3D
29. Organs 3D
Brush up on your anatomy with Organs 3D, which has tens of thousands of positive reviews on Google Play. The nursing app features 3D models, video, audio lectures, quizzes and text to create a rich learning experience for users.
What users are saying:
“I liked it. It gives brief explanation of most internal organs.” “Graphics quality is very low…” “Five stars. This is exactly what I’ve been looking for great 3D image!”
Rating: 
Cost: Free
Available: Google Play and iTunes
 30. Nursing Jokes
30. Nursing Jokes
Nursing is a notoriously stressful profession, and sometimes, what you need most is a lighthearted break from the anxiety. Look to Nursing Jokes on Android for some necessary humor to get you through long shifts.
What users are saying:
“Repetitive. Not enough content and not all that funny.” “Good, funny jokes.”
Rating: 
Cost: Free
Available: Google Play
 31. MediBabble Translator
31. MediBabble Translator
MediBabble is a professional-grade app that provides medical interpretation for healthcare workers and nurses. This app aims to improve safety and efficiency nurses can provide to non-English speaking patients. It aims to allow users to communicate faster, on the go, with those who do not speak English.
What users are saying:
“Very useful…” and “Amazing for gathering information!” Users say the app is “very good for asking patients questions and describing their conditions…”
Rating: 
Cost: Free
Available: iTunes
 32. IDdx: Infectious Diseases
32. IDdx: Infectious Diseases
This app allows users to search by description and lists a number of infectious diseases that could relate to it. It lists symptoms and conditions of diseases to allow for fast recognition and diagnostic support. The searchable component of this app helps users to quickly find vivid images and information so that fast response time is possible. It displays pictures for diagnostics and support for emergency situations.
What users are saying:
“Very fine reference especially with multiple sources integration…” and “Using patient systems was effective for a precise conclusion.”
Rating: 
Cost: Free
Available: Android and iTunes
 33. Skyscape Medical Library
33. Skyscape Medical Library
The SML app is a tool to support diagnostics for physicians and nurses. It pulls from 400 resources from various associations to make finding information easy. Searches by keyword are easy and highly effective. A total everything-you-need tool, this app makes it easy to find key information whenever it becomes immediately necessary and you’re on the go.
What users are saying:
“It’s a go-to app for medical information…”
Rating: 
Cost: Free
Available: Android and iTunes
 34. Eponyms
34. Eponyms
Eponyms features hundreds of common and obscure medical eponyms for easy searching and verification. It allows users to quickly look up the meaning of a term, no matter how obscure or unique it is, to find out what it refers to. This makes finding information faster than trying to navigate complex medical conditions by limited names.
What users are saying:
“Excellent. Very thorough.” And “”Really nice app, very helpful, but needs more eponyms added…”
Rating: 
Cost: Free
Available: Android and iTunes
- Nursing Central app is available through the Amazon store and is compatible on some Android devices.
- Ratings are based on the current app version for either Google Play or iTunes stores. Ratings are current at the time of publishing.
- For clarity, ratings have rounded to the whole number. Please visit the app store to review the current ratings.
- Some apps may require you to purchase. Some additional costs may also incur after initial payment. Please refer to the app’s terms of service agreement before purchasing.
- Some apps may require you to sign up before using.
- Some free apps may have in-app advertising or purchases.
- Please refer to the app’s compatibility requirements as they may not work on all devices.

 In order to provide top quality care to their patients, Nurses must be focused and alert. Burnout in Nurses is worrisome because common side effects are forgetfulness, impaired concentration, anxiety, and depression. As a Nurse leader you want to make sure patient's lives are in good hands and the Nurses are well.
In order to provide top quality care to their patients, Nurses must be focused and alert. Burnout in Nurses is worrisome because common side effects are forgetfulness, impaired concentration, anxiety, and depression. As a Nurse leader you want to make sure patient's lives are in good hands and the Nurses are well. 


 Smiling is contagious and really the only thing Nurses are okay spreading around. Being happier during your shift usually results in it going by a little faster. I wanted to know how Nurses made their shifts a little more enjoyable. I did some research and here’s what I discovered.
Smiling is contagious and really the only thing Nurses are okay spreading around. Being happier during your shift usually results in it going by a little faster. I wanted to know how Nurses made their shifts a little more enjoyable. I did some research and here’s what I discovered. Jokester, Trini Moad Snow, was a Nurse for over 40 years. She's now retired at age 91 but, talks about her happy days at work and the path to her passion. Moad Snow recalls picking vegetables after high school so she could save up enough money for Nurse training and that one time when she cut off an executive's tie! If you're interested in more of Trini's stories continue reading below.
Jokester, Trini Moad Snow, was a Nurse for over 40 years. She's now retired at age 91 but, talks about her happy days at work and the path to her passion. Moad Snow recalls picking vegetables after high school so she could save up enough money for Nurse training and that one time when she cut off an executive's tie! If you're interested in more of Trini's stories continue reading below.  Two men discuss their career paths in a female dominated work environment, Nursing. Brian Medley and Zain Rehman talk Nursing shortages, specialty options, salary, and more. Read below to find out more about the interview.
Two men discuss their career paths in a female dominated work environment, Nursing. Brian Medley and Zain Rehman talk Nursing shortages, specialty options, salary, and more. Read below to find out more about the interview.  Two professors at USF collaborated to work on improving self-care at home for patients with congestive heart failure. Another goal was to reduce their hospital readmissions. They knew most patients are living on their own after they get out of the hospital and it can be a challenge for patients to keep up with their
Two professors at USF collaborated to work on improving self-care at home for patients with congestive heart failure. Another goal was to reduce their hospital readmissions. They knew most patients are living on their own after they get out of the hospital and it can be a challenge for patients to keep up with their  Nurses are on the move and they aren't carrying around medical books and a computer to help them when they need it. Wait, on second thought, that little smart phone in your pocket is just that, a computer, filled with apps catered to your needs.
Nurses are on the move and they aren't carrying around medical books and a computer to help them when they need it. Wait, on second thought, that little smart phone in your pocket is just that, a computer, filled with apps catered to your needs. 

































 Thankfully Nurse Markey decided to take a different route to pick up her step-kids at school because she ended up at the right place at the right time.
Thankfully Nurse Markey decided to take a different route to pick up her step-kids at school because she ended up at the right place at the right time. After reading this article
After reading this article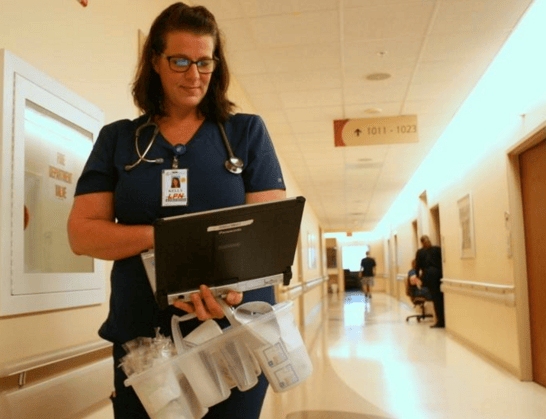 You
You Recently, Indeed.com – a massive job search platform that greets over 200 million monthly visitors – took a look at which cities in the U.S. pay nurses the most while giving them the biggest bang for their bucks. The west of the U.S. – California especially – was overwhelmingly dominant.
Recently, Indeed.com – a massive job search platform that greets over 200 million monthly visitors – took a look at which cities in the U.S. pay nurses the most while giving them the biggest bang for their bucks. The west of the U.S. – California especially – was overwhelmingly dominant.