 Maybe you’re not looking for a new job, maybe you are, or maybe you want to learn more and gain helpful insight and tips about your field. Perhaps you’re thinking about changing your specialty and if you are, do you need to go back to school? The best way to help you with your decision is with an informational interview.
Maybe you’re not looking for a new job, maybe you are, or maybe you want to learn more and gain helpful insight and tips about your field. Perhaps you’re thinking about changing your specialty and if you are, do you need to go back to school? The best way to help you with your decision is with an informational interview.
This article will tell you all you need to know about these interviews to help you get answers and information specific to you and your needs. An informational interview is just what it sounds like – an opportunity for you to learn whether a change is a good fit for you. You have nothing to lose and everything to gain.
Have you ever used an informational interview to move your nursing career forward? Did you know that informational interviews are a form of professional networking?
When you’re seeking a position, doing research on a nursing specialty, vetting a potential employer, or looking to make valuable connections with other healthcare professionals, informational interviews are a vehicle to achieve your goals.
What Is An Informational Interview?
An informational interview is a process by which you request to meet with another professional to learn more about what they do, who they are, the organization they work for, or other valuable information.
These meetings are not about directly asking for a job; however, they are indeed about you meeting with an individual who holds power, connection, influence, or knowledge to which you would like access.
Informational interviews are best conducted in person, but telephone, Skype, or FaceTime are fine if meeting face-to-face isn’t possible.
During such a meeting, you ask prepared questions in order to stimulate conversation while remaining open to new questions that may arise in response to your interviewee’s answers.
Remember that although informational interviews are not actual job interviews, the act of helping an influential professional to learn how valuable you are can sometimes lead to surprising and unexpected outcomes.
How To Ask for An Informational Interview
Request an informational interview in writing, making your intentions very clear. Your introductory letter or email will be somewhat like a cover letter, yet it will not contain a request to be interviewed for a particular position.
In your letter, briefly introduce yourself and give a very short synopsis of your nursing career. Explain your goals and the general information you’re seeking; you can even share your specific questions in advance.
Be sure to inform your potential interviewee right away that you value their time, and offer a potential time limit for the conversation (for example, 30 minutes). If meeting at their workplace, ask to know what favorite treat and beverage you can bring from a nearby café; if you plan to meet at a café or restaurant, be very clear that you’ll be covering all costs.
The Interview Itself
During the interview, be clear, concise, and well-prepared. Bring a notebook and pen, and be sure to have your resume and business card in case they’re requested.
Be certain to smile, laugh, make eye contact, speak eloquently, and practice good listening skills and body language. Express gratitude at both the beginning and end of the meeting. Remember to show curiosity about your interviewee’s life and career, and ask for their professional mailing address and business card before you part ways.
Once your questions have been answered, always ask your interviewee if there is any way in which you could be helpful to them, even if you think there isn’t; the offer is a way of showing a spirit of grateful reciprocity.
Following Up
Always mail a handwritten thank you note within several days of the interview; an email is simply not sufficient. Also, connect with your interviewee on LinkedIn and other social media platforms.
If your connection is a positive one, consider sending a holiday card each year, and check in by email from time to time. If a referral, introduction, or other lead bears positive results, write to inform them and reiterate your gratitude.
An informational interview can be a powerful means to gathering information, receiving introductions, or opening up new opportunities; employ this underutilized networking strategy to stimulate your own career growth.

 When Nurse Tommy Sing answers a patient's call he has to put his game face on, literally. Sing spends his days pushing different buttons on medical machines as well as game controllers. He may want to keep his actual day job though. His patients seem to always beat him.
When Nurse Tommy Sing answers a patient's call he has to put his game face on, literally. Sing spends his days pushing different buttons on medical machines as well as game controllers. He may want to keep his actual day job though. His patients seem to always beat him. 


 Nurses do so much, including laying our heads down to rest during our toughest moments. A hair stylist had the opportunity to turn the tables and let the Nurse do the resting and let her be taken care of. The stylist wanted the Nurse to have no worries and be completely relaxed and safe in her hands at that moment, the same way a Nurse treats a patient.
Nurses do so much, including laying our heads down to rest during our toughest moments. A hair stylist had the opportunity to turn the tables and let the Nurse do the resting and let her be taken care of. The stylist wanted the Nurse to have no worries and be completely relaxed and safe in her hands at that moment, the same way a Nurse treats a patient. 
 How can you properly care for a patient if you don’t understand their personal needs? Communication is key. Making a patient comfortable goes far beyond providing warm blankets. It is about the patient trusting you and knowing you have things in common that show them you understand how they feel and what they need.
How can you properly care for a patient if you don’t understand their personal needs? Communication is key. Making a patient comfortable goes far beyond providing warm blankets. It is about the patient trusting you and knowing you have things in common that show them you understand how they feel and what they need. 

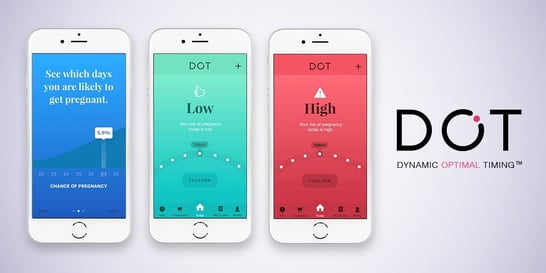 Do you worry about family planning with some of your patients? If so, this article about an “app” that helps to avoid unwanted pregnancies may be helpful. “Dot” is the only family planning app that relies solely on period start dates. Health experts believe an estimated 225 million women worldwide are not using effective family planning methods, but want to avoid pregnancy.
Do you worry about family planning with some of your patients? If so, this article about an “app” that helps to avoid unwanted pregnancies may be helpful. “Dot” is the only family planning app that relies solely on period start dates. Health experts believe an estimated 225 million women worldwide are not using effective family planning methods, but want to avoid pregnancy. We need a Wednesday feel good story and this is a terrific one!
We need a Wednesday feel good story and this is a terrific one!  “We were just praying that Hudson wouldn’t suffer any effects from the surgery and as far as we can tell he is one perfectly health little boy,” she says.
“We were just praying that Hudson wouldn’t suffer any effects from the surgery and as far as we can tell he is one perfectly health little boy,” she says.
 Maybe you’re not looking for a new job, maybe you are, or maybe you want to learn more and gain helpful insight and tips about your field. Perhaps you’re thinking about changing your specialty and if you are, do you need to go back to school? The best way to help you with your decision is with an informational interview.
Maybe you’re not looking for a new job, maybe you are, or maybe you want to learn more and gain helpful insight and tips about your field. Perhaps you’re thinking about changing your specialty and if you are, do you need to go back to school? The best way to help you with your decision is with an informational interview.  If you’re a parent, you know how daunting those first few months are, not to mention exhausting. Many of you work with new mothers in the maternity ward, doctor’s office, etc. Wouldn’t it be helpful to offer more education about SIDS and how to care for a newborn?
If you’re a parent, you know how daunting those first few months are, not to mention exhausting. Many of you work with new mothers in the maternity ward, doctor’s office, etc. Wouldn’t it be helpful to offer more education about SIDS and how to care for a newborn? Washington DC area philanthropists Joanne and Bill Conway have committed to a $5 million gift to support our CNL program, funding the education of more than 110 new nurses over five years, beginning in 2018. The Conways, who gave a similar gift to UVA Nursing in 2013 are, with this transformative gift, renewing their pledge to encourage a broader diversity in the students who enroll in this program.
Washington DC area philanthropists Joanne and Bill Conway have committed to a $5 million gift to support our CNL program, funding the education of more than 110 new nurses over five years, beginning in 2018. The Conways, who gave a similar gift to UVA Nursing in 2013 are, with this transformative gift, renewing their pledge to encourage a broader diversity in the students who enroll in this program. All Conway Scholars (entering this summer `17, to graduate in 2019) receive a year-long grant for tuition and related expenses ($24k over the year). The new gift, which will begin funding students in 2018
All Conway Scholars (entering this summer `17, to graduate in 2019) receive a year-long grant for tuition and related expenses ($24k over the year). The new gift, which will begin funding students in 2018 A new cervical cancer study found that women with hysterectomies weren't accounted for in the previous study of cervical cancer death rates. The new evidence shows the death rate is 10.1 per 100,000 black women and 4.7 per 100,000 white women.
A new cervical cancer study found that women with hysterectomies weren't accounted for in the previous study of cervical cancer death rates. The new evidence shows the death rate is 10.1 per 100,000 black women and 4.7 per 100,000 white women.