Contributors: Maria R. Shirey, PhD, MBA, RN, NEA-BC, ANEF, FACHE, FAAN via www.americannursetoday.com

For leadership to be authentic, programs should focus on both external programming and individual improvement. The most important factor of individual improvement is self-awareness. Authentic leadership on an individual level can be measured by an Authentic Leadership Questionnaire (ALQ).
In 2013 alone, U.S. organizations spent more than $15 billion on leadership development activities. Although much of these expenses focus on external programming, including face-to-face workshops, webinars, and e-learning, fewer resources target the internal development of leaders. To maximize sustainable leadership development, emphasis must be given to both external programming and individual improvement.
Experts in the field argue that organizations can more effectively redeploy billions of training resources by focusing on helping leaders mine their regularly scheduled lives for deep insights, feedback, strategies, and solutions. By investing in self-awareness and reflective practices, individuals have a better chance to grow as emotionally capable leaders. This article discusses self-awareness as a means to boost authentic leadership, an emotionally capable positive leadership style, and provides suggestions for enhancing self-awareness.
Self-awareness in authentic leadership
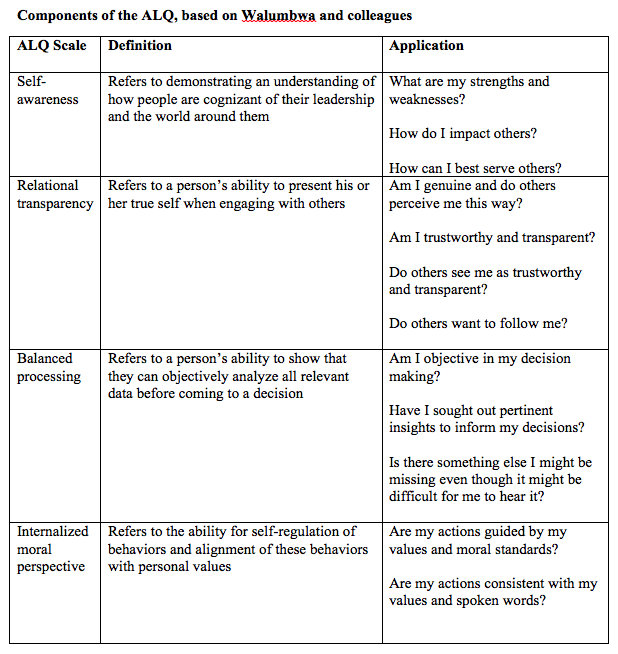
Authentic leadership is a pattern of leader behavior that draws upon and promotes both positive psychological capacities and a positive ethical climate. Elements of this definition are incorporated in the Authentic Leadership Questionnaire (ALQ) developed in 2007 and considered the definitive valid and reliable instrument to measure individual-level authentic leadership.
The ALQ uses four scales to evaluate key components of AL: self-awareness, relational transparency, balanced processing, and internalized moral perspective. (See Components of the ALQ, based on Walumbwa and colleagues.)
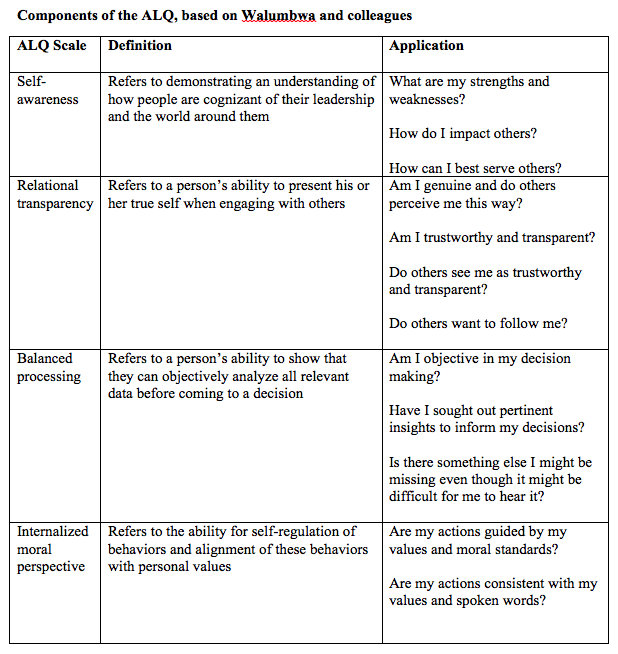
Self-awareness, the focus of this article, refers to an individual’s capacity to show an understanding of personal strengths, weaknesses, and impact on others. In addition to being a core element of authentic leadership, self-awareness is a key component of emotional intelligence that contributes to self-regulation and leader effectiveness.
Enhancing self-awareness
Authentic leadership can be developed. To become an authentic leader, however, requires that individuals pursue a journey of self-discovery, self-improvement, reflection, and renewal. The following recommendations offer direction for building self-awareness in your authentic leadership development journey.
Explore personal strengths and fatal flaws.
Understanding personal strengths helps to maximize potential. Although it’s your strengths that likely got you noticed as a leader, it may not be your strengths that will keep you on track. For this reason, it’s important to also recognize your major weaknesses or fatal flaws so you can minimize these and prevent them from derailing your leadership.
Completing the Strengths Finder instrument and reading about Goldsmith’s identified fatal flaws can help emphasize personal strengths without ignoring major weaknesses. Goldsmith defines fatal flaws as bad behaviors and cites examples of career derailing behaviors such as making destructive comments, withholding information, and claiming undeserved credit.
Understand your limitations and seek others to complement you and the team.
Self-awareness includes understanding personal limitations and acknowledging what still needs to be learned. Self-awareness also involves recognizing the strengths and fatal flaws in others to build a high performing team where all members complement each other and maximize the whole.
Examine emotional intelligence.
Emotional intelligence (EI) refers to people’s ability to recognize and understand their emotions and those of others. With EI, individuals can use their emotional awareness to manage personal behavior and relationships. EI has four distinctive components that need development: self-awareness, self-management, social awareness, and relationship management.
To better understand where you rate on the various EI scales, complete the simple and inexpensive Emotional Intelligence 2.0 instrument. Taking into account results of the assessment as well as suggestions for improvement can guide a personal AL development plan to develop EI.
Observe yourself and engage an observational partner.
Taking the time to record your major decisions along with the rationale for those decisions provides for personal analysis. In looking at the outcomes of decisions, you can establish a personal feedback loop that reveals what went well, what could be done better, and what patterns of behavior may be fruitful or counterproductive.
Including a trusted colleague or coach as an observational partner can offer just-in-time advice or retrospective validation with constructive direction. When leaders ask for input, it’s most beneficial for them to listen to feedback without justifying their actions or retaliating against the invited messenger.
Create down time for daily reflection.
Taking planned down time in the course of a busy schedule helps clear the mind and provide balanced perspective. This activity can involve taking a daily walk, engaging in mindfulness meditation, or reading daily scripture. Reflective down time is needed to enhance self-awareness and to cultivate authenticity.
Dig deep to gain insight.
It’s important for current and aspiring leaders to be able to ask and answer important questions such as: Who am I? What are my values? What is my purpose? What drives me? Are my actions consistent with what I value? How do others see me and is this consistent with how I wish to be seen?
Digging deep to honestly explore these questions requires time, dedication, and possibly validation from others. This type of deep reflection represents the inner work of leadership development that someone else cannot do for you.
Keep a reflective journal.
Keeping a journal helps to record personal thoughts that can lead to a higher degree of self-awareness and enhance both writing and emotional fluency. In recording daily reflections, this can help to recognize desirable as well as undesirable patterns of emotions and behavior that could either be repeated or modified for self-improvement.
A reflective journal also helps you begin to compose your individual life story, which can shed light on where you have come from, how you have learned from experiences, and provide direction for the future you wish to pursue.
Incorporate time for personal renewal and celebrate milestones.
Taking time to celebrate milestones is important for closure as well as for personal renewal. Pausing at regular intervals can be both inspiring and energizing for yourself and the team you lead.
Authentic leadership journey
Authentic leadership begins with self-awareness. Growing in self-awareness, however, entails individual responsibility, hard work, and devotion to reflective practices. You can use the suggestions in this article to build self-awareness that in turn enhances a personal authentic leadership development journey.
 According to projections from the Bureau of Labor Statistics by 2022 there will be an increase in the number of Registered Nurses of 526,800. That is over half a million! This means lots of nursing jobs for the near future– definitely a career with good prospects. If you are curious about RN salaries this infographic will be helpful.
According to projections from the Bureau of Labor Statistics by 2022 there will be an increase in the number of Registered Nurses of 526,800. That is over half a million! This means lots of nursing jobs for the near future– definitely a career with good prospects. If you are curious about RN salaries this infographic will be helpful.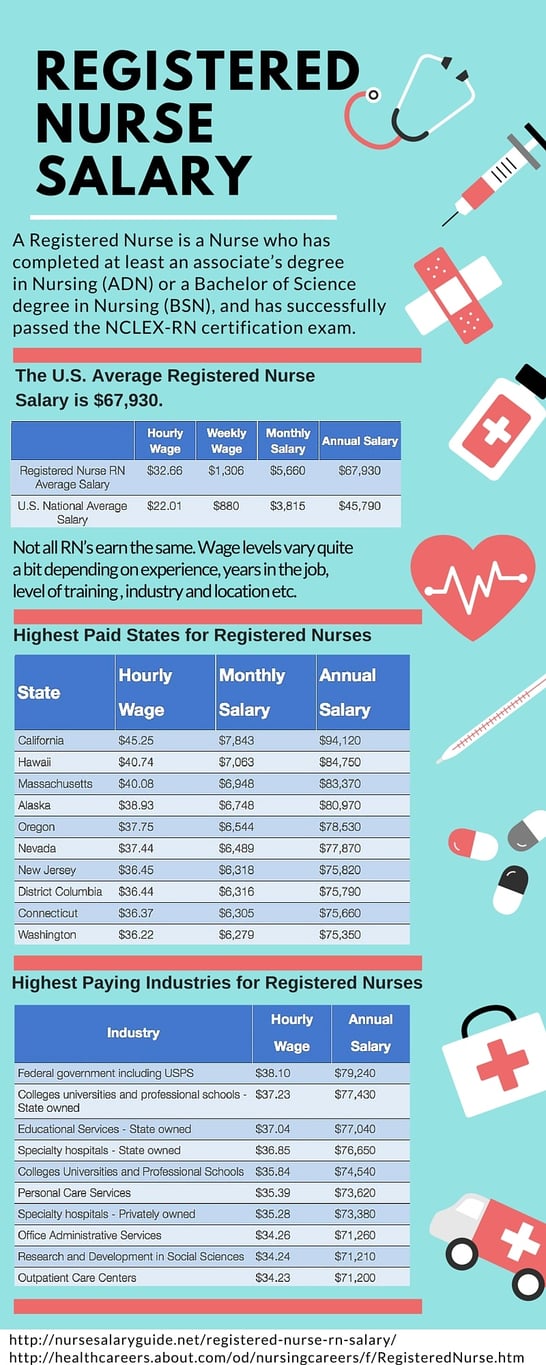



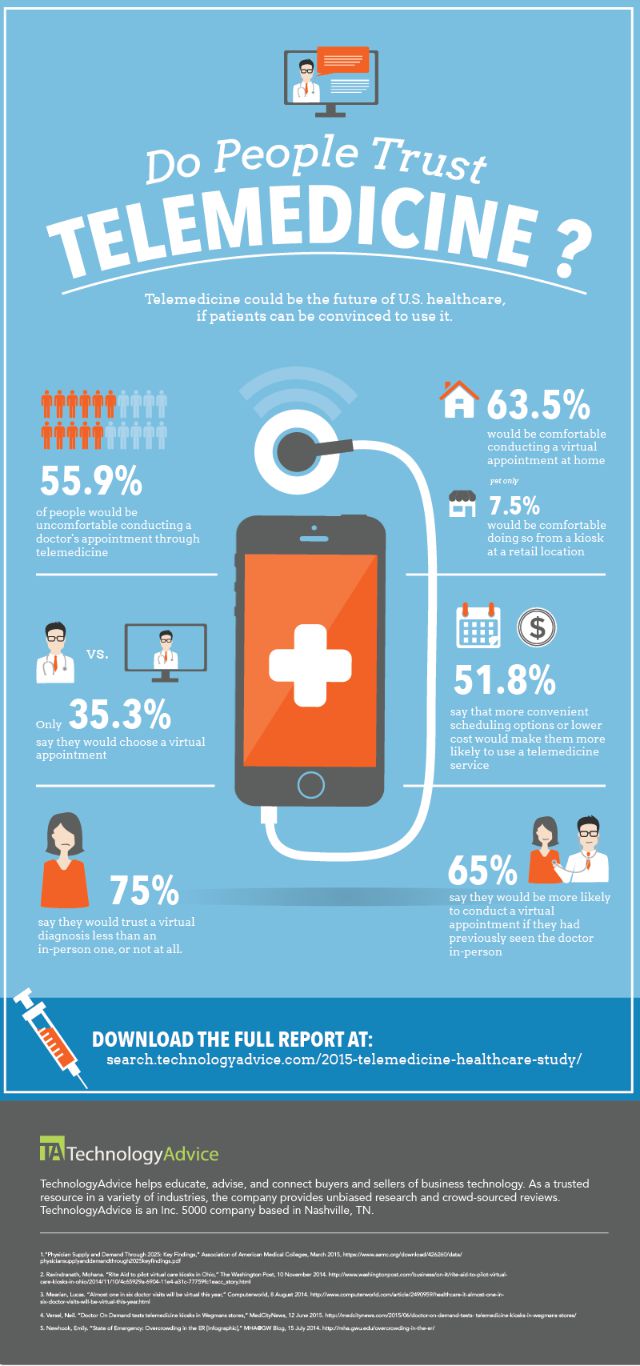
 It is clear that digital technology has a firm grasp on our lives and is advancing daily. We walk around with a computer in our pocket (cellphones) full of endless amounts of information. This technology has changed the way we provide healthcare and with this change there are pros and cons. Specifically, Electronic Health Records (EHRs) or Electronic Medical Records (EMRs).
It is clear that digital technology has a firm grasp on our lives and is advancing daily. We walk around with a computer in our pocket (cellphones) full of endless amounts of information. This technology has changed the way we provide healthcare and with this change there are pros and cons. Specifically, Electronic Health Records (EHRs) or Electronic Medical Records (EMRs). 















 Whistleblowers fear retaliation and the chance that nothing will be done with the information they've provided. An organization's culture should make it's employees feel safe when reporting something. But, there are still times when Nurses refrain from whistleblowing because their work culture has encouraged them not to do so. This delicate area of policy and ethics is a work in progress. As a healthcare worker, what steps do you think would help the process of reporting questionable practices?
Whistleblowers fear retaliation and the chance that nothing will be done with the information they've provided. An organization's culture should make it's employees feel safe when reporting something. But, there are still times when Nurses refrain from whistleblowing because their work culture has encouraged them not to do so. This delicate area of policy and ethics is a work in progress. As a healthcare worker, what steps do you think would help the process of reporting questionable practices?