 You must take the time to read this article! If ever there was a tribute to Nurses, this is it! This story is written by an oncology patient who pays wonderful tribute to many Nurses, but also a particular Nurse who took care of her and helped her get through her surgeries and treatments. I think most patients feel this way about the Nurses that take care of them. They don’t always show their appreciation, but this patient took the time to write about her experience. I hope this will make your day.
You must take the time to read this article! If ever there was a tribute to Nurses, this is it! This story is written by an oncology patient who pays wonderful tribute to many Nurses, but also a particular Nurse who took care of her and helped her get through her surgeries and treatments. I think most patients feel this way about the Nurses that take care of them. They don’t always show their appreciation, but this patient took the time to write about her experience. I hope this will make your day.
RELATIONSHIPS WITH NURSES can stick with patients for the rest of their lives. From nurses, I learned the power of accompaniment. One held my hand as I uncontrollably teared up before port surgery. Another nurse on the oncology floor, when she found out that my husband and I had been married two weeks before I had checked into the hospital, made me a pillow adorned with our wedding pictures. Another shaved my head for me when my hair started falling out at an unsightly pace. A patient-care technician—what used to be called a nursing assistant—held me while I threw up in the bathroom after a two-hour MRI.
Though I don’t like to remember these things, I feel deep gratitude for the nurses who were there with me during painful and sorrowful days. In Siddhartha Mukherjee’s The Emperor of All Maladies: A Biography of Cancer, he quotes journalist and breast-cancer patient advocate Rose Kushner. “Few doctors in this country seem to be involved with the non-life-threatening side effects of cancer therapy,” Kushner notes. “In the United States, baldness, nausea and vomiting, diarrhea, clogged veins, financial problems, broken marriages, disturbed children, loss of libido, loss of self-esteem, and body image are nurses’ turf.”
Although I respected my oncologists for the important role they played in my cancer treatment, I found the wide and varied “turf” that exceptional nurses cover astounding.
A year ago last May, I was checked into Boston’s Beth Israel Deaconess Medical Center (BIDMC) as a 29-year-old non-Hodgkin lymphoma cancer patient just out of spinal surgery and unsure if I’d be able to walk again. A few days post-surgery, two nurses held me next to my hospital bed to see if I could stand. Although I was frightened, I particularly remember Neely Beaulac, R.N., joking with me in her thick Boston accent while I slowly tried to march in place with feet that moved like cinderblocks. Somehow, I broke into a small smile and laughed as Neely cheered me on.
Nearly a year later, I walk the 1.1 miles to the BIDMC from my apartment, stroll into the ’80s-style lobby, and wait in a herd of visitors to ride the elevators to the upper floors. I had planned to meet Neely after her shift. I wanted to interview her about working as an oncology nurse. But when one of her patients had an allergic reaction to a transfusion, she asked if we could meet at the outpatient clinic instead in order to be nearby in case her patient needed her.
While in the elevator, I remember my own allergic reaction to a transfusion, which made my eyes puff up to the size of bouncy balls. Given the complexity of cancer treatment and the series of patient issues that arise moment to moment, the end of an oncology nurse’s shift can be fluid.
“Sorry to make you come here!” Neely says with an incandescent smile. I greet the other staff I know, and the two of us head to a break room to sit and talk. She puts a small bottle of water in front of me, as she has so many times before.
Neely is in her mid-thirties with clear blue eyes and dark hair. She’s attractive in that cool-girl way that makes you want to know her jokes. When she’s doing her job, she can be efficient and quick but also chatty. She makes her nursing tasks look easy yet precise. She’s the kind of nurse who makes a note of when your IV bag is going to run out so you’re not repeatedly awoken by a beeping apparatus. She’s at home barging into a room to restore order. The blue shirt of her scrubs matches her eyes and is adorned with a flowered nametag and a pin a patient gave her, a take on the Superman insignia.
Neely was born for nursing. She tells me her mother would describe her as bossy, organized, particular, “and just that little bit defiant.” Even as a child, she always liked “to be a little helper.” If she thinks she can help by providing information, she wastes no time telling a patient the truth of the matter. She doesn’t sugarcoat.
Once when a consult team visited my room to inform me of a drug called Lupron, used to protect ovaries during chemo, they called it a quick shot in the arm. Neely’s eyebrows furrowed. As soon as the doctors left, she told me, “It’s not a quick shot in the arm, it’s actually a pretty large shot in the tush.”
But for all her native bossiness and helpful bluntness, she says nursing has changed her: “I’m definitely still organized, but I’m not as uptight, not as intense.” She has become better at listening rather than convincing. When frustrated and overwhelmed patients say they want to stop cancer treatment, not an infrequent occurrence, Neely now tries to hear them out, helping patients feel they have more control and aren’t being bossed around.
“I’ve come to realize that a lot of times people don’t want to just go home and be left alone and die,” she says. “They want treatment. But they just want to hear they can leave if they want to.”
ACCORDING TO THE Bureau of Labor Statistics’ Occupational Outlook Handbook, important qualities for nurses are attention to detail, critical thinking, communication, compassion, emotional stability, organizational skills, and physical stamina. Nurses spend their days multi-tasking and managing all kinds of people throughout the day, from patients to parents to spouses and doctors. Although they take on many roles throughout a shift, an eye for detail is essential. Oncology nurses administer chemotherapy and other cancer drugs, making sure that “the correct dose and drug are administered by the correct route to the right patient,” as the nursing reference book Cancer Medicine puts it. Too much of the poison can be fatal.
Oncology nurses also take on other more complicated and personal roles. When I was a patient last year, feeling miserable and immobile in a hospital bed, saltine crumbs were scattered all over the bedtable. I had not asked my husband to clean it, because I was tired of asking him to do things, and I figured crumbs were the least of my worries. Neely then came into my room, and before leaving, wiped down my table. It wasn’t part of her job; she just did it. I felt comforted by someone willing to blur the lines between professional nursing responsibilities and basic human-to-human caregiving, as if going out of her way is not out of her way at all.
“I never want anyone to feel like they’re imposing on me or to say sorry I’m keeping you,” she says. “You’re keeping me?” she pretends to ask a patient while talking to me. “I’m going home…I know you’d rather be anywhere but here.”
Not only do nurses do small things to give you dignity, like picking up crumbs or wiping your mouth, they also clean up filthy messes to restore livable conditions for their patients. One night early in my treatment, my husband and I had friends visiting. As I began falling asleep and my husband was saying goodbye to the friends in the hallway, I had a late onset of nausea from the chemo drugs. Before anyone knew what was happening, I was throwing up my dinner without being able to get off my hard neck brace. In what seemed like seconds, nurses rushed in to clean me off, change my sheets, and generally get the room back in order as if the disgrace had never happened.
Those nurses’ NASCAR crew-like handling of my soiled room helped me move past such a gross and miserable situation more quickly. While receiving cancer treatment and undergoing several surgeries, I encountered numerous take-charge, warm, nursing souls who literally ran toward problems rather than away from them.
And oncology nurses don’t just keep things orderly; the great ones boss people around in both clandestine and overt terms to get the best outcomes for their patients. When I was Neely’s patient, she would gently boss around my husband. “Don’t forget to pack her underwear!” she would remind him, when I had to stay in the hospital longer than expected and he’d rush home to bring me more T-shirts and yoga pants. “Husbands always forget underwear. I don’t know why that is,” she tells me during our recent interview.
Good nurses chase down doctors, assert their opinions based on their sometimes superior knowledge of a situation, and appease family members and other caregivers. Once my discharge was postponed for 48 hours by the attending doctor who barely seemed to have read my file and was rarely available. I felt I could not spend one more day in the hospital with its scratchy sheets, bad food, being woken up every few hours for vital signs, no chance of getting outside into the light of day, institutional showers, and daily injections. It was a nurse who listened to my husband’s rising anger throughout the day as he saw how my mental state was deteriorating. The nurse didn’t have the power to discharge me, but sought out answers from the doctor time after time, despite having a list of patients in equal or worse predicaments.
Oncology nurses are masters at balancing the tensions between patients and doctors, family and treatment team, all the while remaining upbeat and encouraging. Of her tireless questioning of doctors, Neely shrugs and laughs. “What’s the worst they’re going to say? No? And I’ll ask again, ask someone different. And sometimes you never get the answer you want, but at least you feel like you tried.”
BEFORE SHE KNEW so much about the packing tendencies of husbands or the best ways to get patients discharged, Neely wanted to be a teacher. In fact, she went to college for teaching. She had considered nursing, but felt teaching sounded “less stressful and more fun.” During her junior year of college, her cousin had a car accident, and she went to San Diego for the summer to help him around the house and take him to medical appointments. She was inspired by the nurses that cared for him and could see the tangible and emotional difference they made. “That intrigued me,” she says.
Six months before graduating with a degree in teaching, while gaining experience in schools, Neely decided working in a school system wasn’t for her. “I love spending time with children,” she says now, but the built-in tension between teachers and parents and the regiment of teaching to tests didn’t appeal to her. “It wasn’t as fun as I thought,” she admits, even though her parents told her to stick with it.
Just six months after graduation, she had her way and got into nursing school at a two-year program at Labouré College in Dorchester, Massachusetts. After a semester of science courses, she could then start working in hospitals as a floating patient-care technician (PCT). First she gained experience as a PCT in Beth Israel Deaconess Hospital’s Needham outpatient center, and then at BIDMC’s main campus in Boston in an oncology inpatient unit, where I met her and where she has been for more than ten years.
Neely says she’s had no doubts about her profession since graduating from nursing school and has found oncology nursing especially intimate. Instead of patients coming in to be “fixed” and then put on their way, in oncology units, patients often stay for days or weeks, or come back repeatedly for treatment or follow-up in an outpatient clinic. Nurses know everyone’s name and usually the names of many family members or friends. “You want to put a lot into it,” she says, “because you know [your work] really affects people.” Getting to know someone as a person instead of “just a body,” in her words, does make a difference. I can testify.
Each day she’s on the inpatient unit, Neely tries to give patients a goal to improve or maintain their mental state. “Every patient needs a goal for the day, whether that’s to get out of bed, or to go home, or to visit with family,” she says. When she starts her inpatient shifts, she tries to check in with each patient to set a goal and ask, “OK, we have 12 hours, we need to get this done, how do you want to do it?” And on the inpatient floor, she’s up front about how few choices there are for patients. “It’s not rainbows and sunshine. Let’s be real,” she says.
On some days, I remember my goal was to have a bowel movement or to get from the bed to the chair. “Hopefully by the end, you’re getting out of your chair and doing a few laps [in the hallway] before you go home,” Neely tells me in our interview.
Another of her daily exercises is to put herself in the shoes of others: “I feel like if this were me, what would I do? If this were my husband, my father, what would I do? That’s what it comes down to.”
SEVERAL STUDIES HAVE SHOWN that workplace stress for an oncology nurse can lead to compassion fatigue and burnout that’s caused by just this kind of effort to help others. One 2010 study on oncology nurses, done by Washington University Medical Center in St. Louis, measured compassion fatigue through surveys that captured data on secondary traumatic stress, burnout, and compassion satisfaction. For the study’s 153 oncology inpatient staff participants, 132 of which were registered nurses, nearly 40 percent were at a high risk for compassion fatigue, while 44 percent of inpatient staff were at high risk for burnout.
But another 2008 study conducted by Beth Perry, a professor at Athabasca University in Canada, found that “exemplary oncology nurses were able to avoid compassion fatigue by creating moments of connection and making those moments matter.” Sometimes small moments are all that’s left.
Neely says that one of the hardest parts of her job “is when you’re giving someone treatment and it’s not benefitting them. When you know you’re prolonging these horrible side effects.” She tells her patients in that situation, “I’ll give you chemo until your last day if that’s what you want, but I just want you to know you’re not gonna get better. So if there’s anything else you wanted to do, get it done. Don’t have me poison you to the very end.”
I ask Neely about how she manages working through life and death situations daily. She admits that other nurses she works with are better at erecting emotional barriers. When one of her patients has a bad outcome, “It still rocks me every time.…I can’t separate myself,” she says. “I’m home praying for these people, I say my prayers every night.”
But even in hopeless times, she still feels she can help. “If you know someone is not going to do well—and ultimately die—because that’s what everyone is afraid of with cancer, the Big C, just give them dignity. If there’s something they want to do, get it done. You want your dog to come in? You want to leave and go wherever? Just help them get that done.” She admits that if she were in that situation, she would most likely want to go home with her husband and dog to die.
Neely’s husband, Jamie, survived testicular cancer before they met, which gives her additional personal insights, but also makes her feel she shouldn’t discuss emotionally difficult parts of her day with him—it would hit too close to home. On the other hand, their joint experiences with the effects of cancer help crystallize their priorities. “There’s a lot that just doesn’t rock us,” she says. “To me, unless someone’s dying, dead, or suffering from extreme illness, I’m like, how stressed out can you be?”
She knows that life can change in a minute. Neely texted me the day after I met with her to say our discussion had made her reflect more deeply on her nursing career. One thing that kept coming to her mind was something that happened to her in college. While on a jog, a car hit her.
“I don’t remember much from that day,” she wrote in the text, “But I do remember I had this nurse who was with me every moment and kept telling me everything is going to be OK.…He was so comforting, and when I decided to go into nursing, he always stuck with me. I always want to give people the comfort that he offered me that day.”
As for me, I’m grateful that I can sit up, reach my computer to type this, and be able to thank Neely for the part she played, alongside many others, in getting me to where I am today. When I do thank her during our interview, she looks me in the eye and insists, “You did it!” Of course she would.

 We’ve all experienced or heard about long wait time to receive medical attention in the Emergency Room. It’s tough on everyone involved – the patients, their families and medical staff. Many people put off going to the emergency room for this very reason. If they can avoid it, they do. Here’s an interesting article about a Canadian study where Nurses are helping to alleviate this situation. Seems to make sense. What are your thoughts about it?
We’ve all experienced or heard about long wait time to receive medical attention in the Emergency Room. It’s tough on everyone involved – the patients, their families and medical staff. Many people put off going to the emergency room for this very reason. If they can avoid it, they do. Here’s an interesting article about a Canadian study where Nurses are helping to alleviate this situation. Seems to make sense. What are your thoughts about it?


 Nurses are always learning. Whether it’s on-the-job with practical experience or continuing your formal education, you are always on a quest to learn more. Perhaps you’re trying to figure out how to do something better, earn your next degree, improve your relationship and listening skills, or how the latest electronic medical records program works. You are determined to move forward and be your best. If you’re looking to advance your formal education, we offer this article as a source of information on Nursing schools and acceptance rates.
Nurses are always learning. Whether it’s on-the-job with practical experience or continuing your formal education, you are always on a quest to learn more. Perhaps you’re trying to figure out how to do something better, earn your next degree, improve your relationship and listening skills, or how the latest electronic medical records program works. You are determined to move forward and be your best. If you’re looking to advance your formal education, we offer this article as a source of information on Nursing schools and acceptance rates.
 If you are a Nursing student wondering what Specialty is right for you, please read on. Perhaps you’re an Experienced Nurse thinking about changing your area of focus. If so, this article is for you too. We hope you find it helpful!
If you are a Nursing student wondering what Specialty is right for you, please read on. Perhaps you’re an Experienced Nurse thinking about changing your area of focus. If so, this article is for you too. We hope you find it helpful! You must take the time to read this article! If ever there was a tribute to Nurses, this is it! This story is written by an oncology patient who pays wonderful tribute to many Nurses, but also a particular Nurse who took care of her and helped her get through her surgeries and treatments. I think most patients feel this way about the Nurses that take care of them. They don’t always show their appreciation, but this patient took the time to write about her experience. I hope this will make your day.
You must take the time to read this article! If ever there was a tribute to Nurses, this is it! This story is written by an oncology patient who pays wonderful tribute to many Nurses, but also a particular Nurse who took care of her and helped her get through her surgeries and treatments. I think most patients feel this way about the Nurses that take care of them. They don’t always show their appreciation, but this patient took the time to write about her experience. I hope this will make your day.

 As our population continues to grow, there are increasing demands on our healthcare system to handle the growth in the number of babies born every year in the US. Do we have enough physicians and midwives to handle the demand for medical services? The answer is No, we don’t. If you’re in a major city, the chances of receiving good maternal healthcare increases, but for those in rural areas, it’s becoming very difficult.
As our population continues to grow, there are increasing demands on our healthcare system to handle the growth in the number of babies born every year in the US. Do we have enough physicians and midwives to handle the demand for medical services? The answer is No, we don’t. If you’re in a major city, the chances of receiving good maternal healthcare increases, but for those in rural areas, it’s becoming very difficult. Think you need to
Think you need to 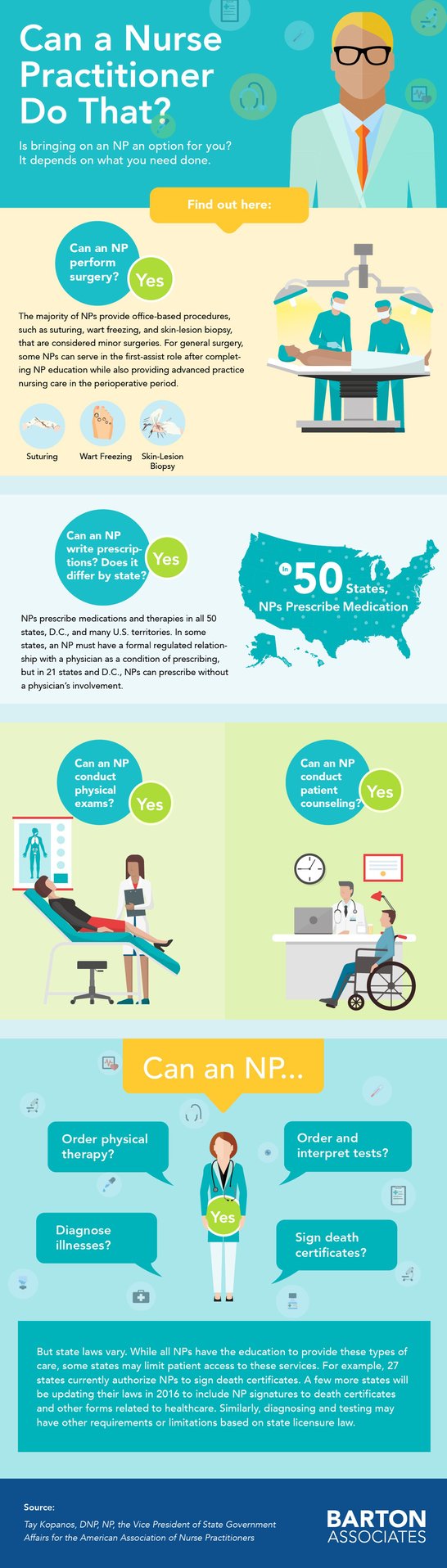
 Brain training with virtual reality systems and robotic exoskeletons are helping paraplegic patients regain some sensations and possibly mobility. Brain-machine interface is changing diagnoses from complete to partial paralysis.
Brain training with virtual reality systems and robotic exoskeletons are helping paraplegic patients regain some sensations and possibly mobility. Brain-machine interface is changing diagnoses from complete to partial paralysis. We here at DiversityNursing.com are looking for a variety of topics that we hope you’ll find interesting. Is this article about new bundled payments models something that is helpful and informative for you? Please let us know your thoughts.
We here at DiversityNursing.com are looking for a variety of topics that we hope you’ll find interesting. Is this article about new bundled payments models something that is helpful and informative for you? Please let us know your thoughts.
 In this day and age, you probably think women don’t die in childbirth, and if they do, it must be an extremely rare occasion or in 3
In this day and age, you probably think women don’t die in childbirth, and if they do, it must be an extremely rare occasion or in 3 United States dropped from 607.9 deaths per 100,000 births in 1915 to 7.2 in 1987. But over the past 30 years, the maternal mortality rate trend reversed and steadily marched upward.
United States dropped from 607.9 deaths per 100,000 births in 1915 to 7.2 in 1987. But over the past 30 years, the maternal mortality rate trend reversed and steadily marched upward.