 The healthcare industry is filled with challenging and rewarding job opportunities. For those who are actively pursuing a career in nursing and who eventually wish to acquire leadership roles in that field, striving for the occupation of Chief Nursing Officer is a worthwhile endeavor. To be a successful CNO in the healthcare system there are specific requirements, qualities, and skill sets that the industry requires of their employees. These attributes can determine the likelihood of potential employment. Along the same vein, what does it really take to become a good CNO (Chief Nursing Officer) in the medical sector?"
The healthcare industry is filled with challenging and rewarding job opportunities. For those who are actively pursuing a career in nursing and who eventually wish to acquire leadership roles in that field, striving for the occupation of Chief Nursing Officer is a worthwhile endeavor. To be a successful CNO in the healthcare system there are specific requirements, qualities, and skill sets that the industry requires of their employees. These attributes can determine the likelihood of potential employment. Along the same vein, what does it really take to become a good CNO (Chief Nursing Officer) in the medical sector?"
Basic Requirements
The requirements for the role of CNO vary depending on the preferences of the employer. There is, however, a general consensus that to be considered for the position of CNO, the applicant needs years of nursing experience and some form of a graduate degree. Some hospitals or medical affiliates require as little as 5 years of experience while others require applicants have 7 - 10 years of practice in the medical industry. The CNO position is the highest ranking Nurse in administration and that role is not taken lightly.
Taking the right educational journey to a specific career is important. The value and focus a Chief Nursing Officer hopeful applies to their education path speaks volumes to potential employers. Having a MS Nursing (management and organizational leadership) degree, a MS in Nursing (leadership in health care systems) degree or a Master of Science in Nursing Administration is a common trend among current Chief Nursing Officers. Earning a combination of a science-oriented Nursing degree along with a business emphasis degree is encouraged when seeking a leadership position in healthcare.
If a healthcare employee is seeking admission into a Master's degree program to aid them in their journey toward career advancement, they have expectations to meet. Those in the Nursing field are required to have an active RN license, a Bachelor's degree, and should be aware that RN clinical experience bears heavily in the admissions process. While there are many technical aspects to attaining the title of CNO, becoming a "good" CNO goes beyond the basic requirements.
10 Qualities of a CNO
- Has a passion for fulfilling a leadership role
- Desires to be a positive mentor
- Exhibits a conscious concern for patient care
- Focuses on quality and safety
- Enjoys implementing strategies to solve existing problems
- Decisively initiates responses to emergencies
- Displays commitment and the highest level of competency
- Is a proactive force in a hectic environment
- Exudes compassion and dependability on a daily basis
- Has a keen sense for business matters and has developed organizational skills
Skill Sets of a Good Leader
Chief Nursing Officers realize the importance of setting long and short term goals for the betterment of their facility. As a consummate problem-solver, the business-minded and client-conscious leader balances passion for patient welfare with administrative management. Implementing processes that ensure the business side of healthcare runs smoothly, the leadership role of a CNO is fraught with responsibility, but also with rewards. They are the faculty informers, the interviewers, the proficiency job monitors for Nurses, staff schedulers, and that is just the start to their long list of duties.
Boasting of better pay, job security, and intrinsic rewards, there are many reasons why a CNO values their many-faceted position. Leaders are born through adversity, and a confident Chief Nursing Officer can handle with marked professionalism, the many conflicts that come their way. A good CNO values people and the efficient processes that bring order to chaotic environments.
Any Chief Nursing Officers looking to grow diversity in their facility can click below for contact information. We would be more than happy to help you.



 Being able to read, write, and speak a second language is a highly desired skill in almost every career. However, being a Multilingual or Bilingual Nurse within the healthcare industry has some exceptionally high benefits that make such skilled individuals a prized asset to any team.
Being able to read, write, and speak a second language is a highly desired skill in almost every career. However, being a Multilingual or Bilingual Nurse within the healthcare industry has some exceptionally high benefits that make such skilled individuals a prized asset to any team.

 Technology has made people's lives much easier. There are specialized apps for almost everything and everyone. Some very helpful technology exists for Nurses designed to make your life easier. Here’s the 2015 Top 10.
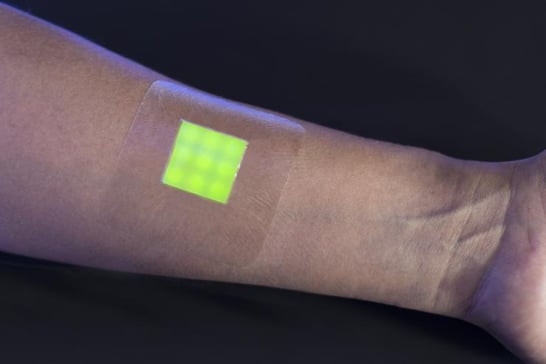
Technology has made people's lives much easier. There are specialized apps for almost everything and everyone. Some very helpful technology exists for Nurses designed to make your life easier. Here’s the 2015 Top 10.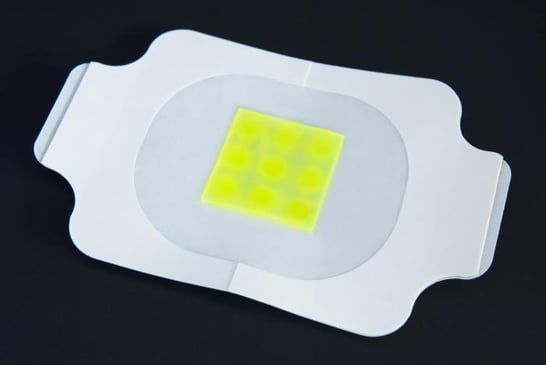 How can you tell if a burn wound has become infected? Wouldn’t it be great if a new technology can alert you to an infection without having to remove the bandage? Scientists in the UK are in the development phase of a bandage that changes color to alert you to an infection. As you know, antibiotics are often prescribed to help stave off infection, however this new technology may help prevent the need for antibiotics.
How can you tell if a burn wound has become infected? Wouldn’t it be great if a new technology can alert you to an infection without having to remove the bandage? Scientists in the UK are in the development phase of a bandage that changes color to alert you to an infection. As you know, antibiotics are often prescribed to help stave off infection, however this new technology may help prevent the need for antibiotics.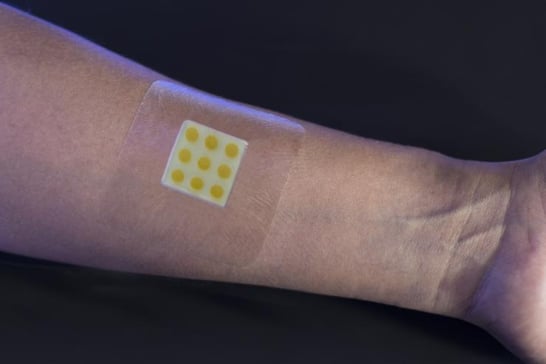
 If you’re feeling unappreciated, read this story to know that many people very much appreciate what you do. They’re not always very good at expressing themselves in a positive way. But most of you understand your patients feelings because as this husband explains, they’re going through one of the worst days of their lives. Many of my friends are Nurses and they are awesome just like you, Every Day.
If you’re feeling unappreciated, read this story to know that many people very much appreciate what you do. They’re not always very good at expressing themselves in a positive way. But most of you understand your patients feelings because as this husband explains, they’re going through one of the worst days of their lives. Many of my friends are Nurses and they are awesome just like you, Every Day.
 If you’re thinking about continuing your education, this article offers some important questions to consider in helping you decide if an online program will accomplish what you want to achieve. We all know continuing your education, if at all possible both financially and personally, will enhance your career, your life and your earning potential.
If you’re thinking about continuing your education, this article offers some important questions to consider in helping you decide if an online program will accomplish what you want to achieve. We all know continuing your education, if at all possible both financially and personally, will enhance your career, your life and your earning potential.
 It seems that Google is involved in just about everything these days! Here’s the latest announcement. The American Heart Association is teaming up with Google on a project for heart health and conquering heart disease. Hopefully their huge investment will yield some promising results for everyone.
It seems that Google is involved in just about everything these days! Here’s the latest announcement. The American Heart Association is teaming up with Google on a project for heart health and conquering heart disease. Hopefully their huge investment will yield some promising results for everyone. More accurate due dates are something both mother and medical professionals want. But is it something possible to achieve? Ultrasound scans are helpful but they can only give an estimate date.
More accurate due dates are something both mother and medical professionals want. But is it something possible to achieve? Ultrasound scans are helpful but they can only give an estimate date.  Nurses have heard it before, "Can you not talk about gross stuff at the dinner table?" But Nurses can't help it when the most disgusting things are completely normal in their everyday lives. They become desensitized to topics like body fluids, infections, and smells and sounds.
Nurses have heard it before, "Can you not talk about gross stuff at the dinner table?" But Nurses can't help it when the most disgusting things are completely normal in their everyday lives. They become desensitized to topics like body fluids, infections, and smells and sounds.