 This story is about a Nurse who worked in oncology and then decided to do palliative care in people’s homes. She finds it an honor to be with the patient and their family during the last few days of the patient’s life. She notes how the patient is much more in control and comfortable at home than they are in the hospital and wonders if there’s a way to do it better in the hospital. She has learned to be honest with the patient’s family if they ask if their loved one is dying. She has found they ask, because they really want to know, to prepare themselves. If you are not a palliative care Nurse, is it something you would consider? This story will give you excellent insight.
This story is about a Nurse who worked in oncology and then decided to do palliative care in people’s homes. She finds it an honor to be with the patient and their family during the last few days of the patient’s life. She notes how the patient is much more in control and comfortable at home than they are in the hospital and wonders if there’s a way to do it better in the hospital. She has learned to be honest with the patient’s family if they ask if their loved one is dying. She has found they ask, because they really want to know, to prepare themselves. If you are not a palliative care Nurse, is it something you would consider? This story will give you excellent insight.
Palliative care nurse Theresa Brown is healthy, and so are her loved ones, and yet, she feels keenly connected to death. "I have a deep awareness after working in oncology that fortunes can change on a dime," she tells Fresh Air'sTerry Gross. "Enjoy the good when you have it, because that really is a blessing."
Brown is the author of The Shift, which follows four patients during the course of a 12-hour shift in a hospital cancer ward. A former oncology nurse, Brown now provides patients with in-home, end-of-life care.
Talking — and listening — are both important parts of her job as a palliative care nurse. This is especially true on the night shift. "Night and waking up in the night can bring a clarity," she says. "It can be a clarity of being able to face your fears, it can be a clarity of being overwhelmed by your fears, and either way, I feel like it's really a privilege to be there for people."
Sometimes Brown finds herself bridging the gap between patients who know they are dying and family members who are still expecting a cure. "There can be a lot of secrets kept and silences. ... One thing that palliative care can be really good at is trying to sit with families and have those conversations," she says.
While some might see her job as depressing, Brown says that being with people who are dying is a profound experience. "When you're with people who die ... and being in their homes and seeing their families, it's incredible the love that people evoke. And it makes me realize this is why we're here; this is what we do; this is what we give to each other."
Interview Highlights
On cutting costs and stretching nurses too thin
There's a sense that you can stretch a nurse just like an elastic band and sort of, "Well, someone called off today." That means a nurse calls in and says that she's sick or her car broke down or he won't be there, and sometimes we're able to get someone onto the floor to take that person's place, but often we're not. Or an aide might not be able to show up for whatever reason, and then the assumption is just, "Well, the nurses will just do all the work that the aide would've done," and the problem is that people do not stretch like rubber bands, and even rubber bands will break if you stretch them too far.
On loved ones wanting to feed their dying family members
Food is so fundamental, and their feeling is "I'm letting my husband starve to death and that's wrong." So I have to talk them through the process of the body slowly going in reverse. All the processes we think of as normal and that are integral to life, they're all slowing down. And so the body just doesn't need food when someone gets very close to the end of their life and, in fact, they found that forcing someone to eat can mean that they just have this food sitting in their stomach, they're not able to digest it, can actually make them more uncomfortable. So I talked to [one family member] about that, but tried to do it as gently as possible, while also acknowledging the incredible love that was motivating her and trying to honor that, but make it clear that she needed to show her love by being close with her husband, by holding his hand, by talking to him, but not by feeding him.
On whether patients ask if they're dying
No, they don't. ... I think it's because they're afraid. They want to just take things day by day. I did have a wife once ask me. She said, "You know, I'm not new to this, and I want you to just tell me. Is he dying?" And at that point I was a pretty new nurse and I didn't have the experience to know to say, "Yes." Now I would know to say that. ... I got a sense that she really wanted to know and no one else was telling her. ...
Physicians can have a mindset of "we're thinking positively, we're focusing on the good that can come, and we're not going to talk about 'what if it doesn't work out.' " And they will sometimes pull the nurse aside and say, "What's going on?"
On leaving the hospital setting for palliative care
I love the hospital. I never thought I would leave the hospital, but I left to see patients outside the hospital because in the hospital I feel like we never see people at their best. They feel lousy. We wake them up at night. We give them no privacy. We give them, really, almost no dignity. We tell them what they're going to do when, what they're going to eat when, what pill they're going to take when and no one likes living like that. ... So I wanted to see people in their homes because I thought there's got to be a way we could make the hospital better. Seeing what it's like for patients in their homes I thought would show me that. And I would say overwhelmingly what I've seen is control: People have so much more control when they're in their homes and it should not be that hard to give them back a little bit more control in the hospital.
On traveling to a patient's home
When I started, I thought, "I can't believe I'm doing this. I can't believe I just drive up to these houses and go inside them." I live in Pittsburgh, but it can get very rural feeling actually pretty quickly, and I remember ... going to [a house] that was already through back-country roads and then down a gravel driveway, and I thought: "What am I doing? Am I insane?" And then I went into this house, and this family was so loving and amazing and wonderful, so it was a great education for me not to judge. And I know that my workplace checks out and makes sure that the places we're going are real, so that's comforting, but it's definitely a giant leap of faith, and you just have to make that leap.
On home care versus hospital care
Often in the hospital they can be more comfortable in terms of we're relieving their pain, we're getting them anti-nausea medications very quickly, but ... they're not as comfortable with themselves, and in their homes they seem much more comfortable with themselves and with the people around them, and I had never thought about those two things as being so distinct, but they are. So the question then is how do we give people care that marries those two things, because they're both so important.
On how patients express appreciation to nurses
A very popular gift in my hospital was Starbucks [gift] cards. ... Often people bring in cookies and chocolate and that's wonderful, but I remember one nurse saying, "You know, I wish someone would just bring in a lasagna." ... Because we never have time to eat and then you go into the break room and you're hypoglycemic and you see all this chocolate, and so you eat all this chocolate, which doesn't really help you feel that much better in the long run. So to actually drop off a meal is wonderful.
 As Nurses, a big part of your job is empathy for your patients and their families. You’re so good at understanding what your patients are going through because you care and this I think, is primarily why you decided to become a Nurse – to help people and lend a sympathetic ear. You educate, show compassion, love and understanding every day. You are amazing!
As Nurses, a big part of your job is empathy for your patients and their families. You’re so good at understanding what your patients are going through because you care and this I think, is primarily why you decided to become a Nurse – to help people and lend a sympathetic ear. You educate, show compassion, love and understanding every day. You are amazing! 


 Education, education, education… you’ve heard about the importance of a good education all of your life. It’s right up there with buying a house, where location, location, location is the mantra. This article explains what hospitals and health systems are looking for when hiring Nurses and why a BSN degree or higher is important.
Education, education, education… you’ve heard about the importance of a good education all of your life. It’s right up there with buying a house, where location, location, location is the mantra. This article explains what hospitals and health systems are looking for when hiring Nurses and why a BSN degree or higher is important. 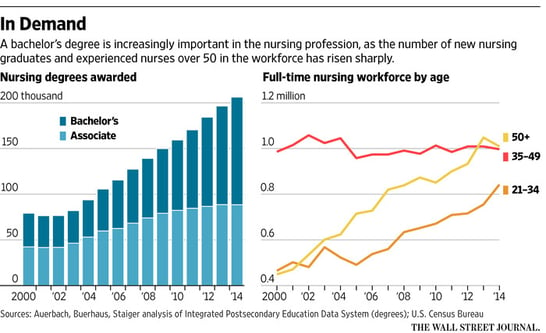

 Are you a leader? Are you someone people look to for advice or to make decisions in a time of crisis? Leaders come in all shapes and sizes. Some are natural leaders, they just know what to do. Others become leaders by observing and learning leadership skills through their mentors or family members. At work, are you someone who leads the way? Do you take a stand when you see something is wrong? We can’t all be leaders, but are there times you just naturally step up to the challenge?
Are you a leader? Are you someone people look to for advice or to make decisions in a time of crisis? Leaders come in all shapes and sizes. Some are natural leaders, they just know what to do. Others become leaders by observing and learning leadership skills through their mentors or family members. At work, are you someone who leads the way? Do you take a stand when you see something is wrong? We can’t all be leaders, but are there times you just naturally step up to the challenge? You work with patients in a medical facility, doctor’s office, perhaps even a school. You do everything you can to keep your patients, yourself and everything around you clean and sterile. After all of the precautions you take, is it possible you are spreading germs? Read on to find out how you can change a step or two of what you’re already doing to prevent further germ contamination.
You work with patients in a medical facility, doctor’s office, perhaps even a school. You do everything you can to keep your patients, yourself and everything around you clean and sterile. After all of the precautions you take, is it possible you are spreading germs? Read on to find out how you can change a step or two of what you’re already doing to prevent further germ contamination. This story is about a Nurse who worked in oncology and then decided to do palliative care in people’s homes. She finds it an honor to be with the patient and their family during the last few days of the patient’s life. She notes how the patient is much more in control and comfortable at home than they are in the hospital and wonders if there’s a way to do it better in the hospital. She has learned to be honest with the patient’s family if they ask if their loved one is dying. She has found they ask, because they really want to know, to prepare themselves. If you are not a palliative care Nurse, is it something you would consider? This story will give you excellent insight.
This story is about a Nurse who worked in oncology and then decided to do palliative care in people’s homes. She finds it an honor to be with the patient and their family during the last few days of the patient’s life. She notes how the patient is much more in control and comfortable at home than they are in the hospital and wonders if there’s a way to do it better in the hospital. She has learned to be honest with the patient’s family if they ask if their loved one is dying. She has found they ask, because they really want to know, to prepare themselves. If you are not a palliative care Nurse, is it something you would consider? This story will give you excellent insight.

 Many Nurses have a 6th sense when it comes to their patients. This story is about a Nurse who’s patient was in a coma after a C-section. Nothing was bringing the patient out of the coma. The Nurse’s actions changed the outcome of could have been a very tragic situation.
Many Nurses have a 6th sense when it comes to their patients. This story is about a Nurse who’s patient was in a coma after a C-section. Nothing was bringing the patient out of the coma. The Nurse’s actions changed the outcome of could have been a very tragic situation.



