
First article written by Frontier Nursing University
Second article Written by Marissa Silver
Frontier Nursing University believes in increasing awareness of the importance of cultural competency and decreasing health disparities. This article is about their 7th annual Diversity Impact Event. FNU states “Diversity Impact is designed to open the door for nurses to foster and strengthen collaborative discussions to address health disparities to improve minority health among underrepresented and marginalized groups.” Enjoy this informative article.
In a rapidly-changing, sometimes divided world, Frontier Nursing University (FNU) emphasizes the value of respecting and honoring diversity.
In the United States, there is a wide gap in health outcomes. Several populations face greater obstacles in obtaining good health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, sexual orientation, physical or mental disability, or geographic location. These disparities may exist because of social and economic inequality, inadequate health care providers or systems, and bias on the part of health care providers or patients.
The gap forming in the health of women before and during pregnancies is also a source of concern. Determinants of a mother’s health may include social factors, ethnic or racial group, or her previous health statu s. An infant child is also impacted by factors such as nutrition, family income, and the geographic location of their homes and neighborhoods.
s. An infant child is also impacted by factors such as nutrition, family income, and the geographic location of their homes and neighborhoods.
Additionally, consider this: women living in rural areas have less access to health care than women living in urban areas. Where 22.8% of women live in what is defined as a “rural” area in the U.S.¹, there is a significant disparity between the health care they receive and the health care received by the “urban” population of women.
Although health care needs around the nation are diverse, health care providers do not reflect the population. In 2008, only 16.8% of Registered Nurses residing in the United States represented diverse racial and ethnic backgrounds². Additionally, underrepresented groups make up less than 10% of nursing school faculty³. The nursing profession faces the challenge of recruiting and retaining a culturally diverse workforce that mirrors the nation's demographics.
With these challenges in mind, it is important that our education system equips nurse practitioners, nurse-midwives and other healthcare professionals with the resources they need to eliminate these disparities, and ultimately achieve health equity.FNU would like to see the Frontier community impact health equity and move forward by uniting through diversity.
On June 1- 4, 2017, Frontier Nursing University held the 7th annual Diversity Impact Student Conference. Diversity Impact is designed to open the door for nurses to foster and strengthen collaborative discussions to address health disparities to improve minority health among underrepresented and marginalized groups. Students will engage in cross-cultural and intercultural workshop activities, along with leadership strategies on current diversity healthcare trends as it relates to patient-provider care.
This year’s Diversity Impact theme is Moving Forward: Uniting Through Diversity. Students will attend sessions hosted by nationally recognized nursing leaders; participate in teambuilding activities, cultural competency awareness training, and open dialogues; network with available FNU students, community leaders, faculty and staff; and learn more about the world with FNU’s International Food Menu.
 Frontier Nursing University conference discusses healthcare diversity
Frontier Nursing University conference discusses healthcare diversity
Factors such as someone's age, race, gender and ethnicity can all play a role in their healthcare.
This weekend, Frontier Nursing University students attended a conference, to learn how those factors and other differences between populations may impact a patient's health and treatment. One factor, which may impact patients in Eastern Kentucky is living in rural communities.
"It's like a totally different population than what you see in urban areas," Vaishu Jawahar who attended the conference said. "Even though we think that sometimes urban populations have it bad, the sheer lack of resources that's out here makes being in a rural area that much harder."
Another topic discussed during the conference was caring for those in the Lesbian, Gay, Bisexual and Transgender (LGBT) community.
"As healthcare providers, no matter what your political views are you have to be able to take care of everyone or at least make them feel comfortable enough to seek out your care," said Jawahar.
As part of the discussion on serving the LGBT community, two Frontier Nursing University students talked about their experience treating patients during last year's mass shooting, at Pulse, a Gay nightclub in Orlando, Florida.
Overall, those who attended the conference said taking the time to get to know the patient and their background can make a difference.
"It's so easy for us to get caught up in our way of life, we forget there's very different realities for everyone," Wilvena Bernard, Diversity Pride Program Coordinator, Frontier Nursing University said.
More than 50 students and faculty attended the conference from across the country.
Last month, University officials announced they are moving student activities from the Hyden campus to Versailles by Fall of 2018.
Interested in learning more about Frontier Nursing University? Check out their Employer Profile! Just Click Here.










 There were many texts, but it was the incomprehensible text encouraging a young man to get back in the truck that sent him to his death. Perhaps you haven’t heard of this story. It started as local news in Massachusetts, but when it went to trial, it became national news.
There were many texts, but it was the incomprehensible text encouraging a young man to get back in the truck that sent him to his death. Perhaps you haven’t heard of this story. It started as local news in Massachusetts, but when it went to trial, it became national news.
 Even though women comprise an estimated
Even though women comprise an estimated  In many cases, patients are now able to access their health care providers through video conferencing, instant messaging, email and other forms of technology. This field, known as telehealth, is growing due to the demand for greater access and convenience in health care, according to
In many cases, patients are now able to access their health care providers through video conferencing, instant messaging, email and other forms of technology. This field, known as telehealth, is growing due to the demand for greater access and convenience in health care, according to 

 Frontier Nursing University conference discusses healthcare diversity
Frontier Nursing University conference discusses healthcare diversity
 Unique challenges encompass the delivery of quality healthcare in the entire world as a whole. People of all ages are terminally ill -- with approximately half the American population fighting hypertension, diabetes, cardiovascular diseases, arthritis and mental related illness.
Unique challenges encompass the delivery of quality healthcare in the entire world as a whole. People of all ages are terminally ill -- with approximately half the American population fighting hypertension, diabetes, cardiovascular diseases, arthritis and mental related illness. Registered nurses are the most frequent point of contact with patients in healthcare. They “provide and
Registered nurses are the most frequent point of contact with patients in healthcare. They “provide and .jpg?width=546&height=410&name=image1%20(1).jpg)


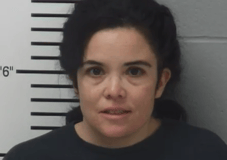 Samantha Rivera from Missouri is being accused of identity theft of a Nurse and using that I.D to get hired at St. Alexis Hospital. Rivera lied about having Nursing experience and a degree. According to
Samantha Rivera from Missouri is being accused of identity theft of a Nurse and using that I.D to get hired at St. Alexis Hospital. Rivera lied about having Nursing experience and a degree. According to  Over in California Nurse imposter, Chad Litz, also with a history of lying, has been arrested. In 2015, the California Board of Registered Nursing
Over in California Nurse imposter, Chad Litz, also with a history of lying, has been arrested. In 2015, the California Board of Registered Nursing  This heartwarming Ted Talk is a glimpse into
This heartwarming Ted Talk is a glimpse into