 As Nurses, death can be a regular, everyday occurrence. But just because we encounter death frequently does not mean that experiencing the loss of a patient won't impact us. In this profession, we care for people when they are at their most vulnerable, and we create meaningful relationships with many of our patients and their families.
As Nurses, death can be a regular, everyday occurrence. But just because we encounter death frequently does not mean that experiencing the loss of a patient won't impact us. In this profession, we care for people when they are at their most vulnerable, and we create meaningful relationships with many of our patients and their families.
When we lose a patient, it’s common for Nurses to experience grief and it can be challenging to navigate the grief you feel. Here are some ways to help you cope with the loss of a patient.
Acknowledge the Loss
Losing a patient is just as real as losing any other person in your life. Try not to minimize the impact the loss of a patient has made on your life. Allow yourself the time to feel your feelings and emotions.
It is normal to experience emotions of sadness, anger, shock, or even disbelief. Some Nurses may also experience physical changes in response to the loss, such as trouble sleeping, nausea and fatigue, anger, or poor concentration. Acknowledging the loss and honoring the person's life can help you move past your grief.
Find Support
Finding support from your peers, colleagues, friends, and family is essential for coping with the loss of a patient. Having a good support system allows you to express your feelings of grief and helps you get some of the emotions you are experiencing off your chest.
For example, many facilities offer briefings after a patient is lost so that all healthcare team members can express their thoughts and feelings and discuss how to improve patient care in the future. In addition, some Nurses may find that speaking with a therapist or grief counselor can help them navigate feelings and offer support after experiencing the loss of a patient.
Practice Self-Care
Grief can often manifest itself physically, so it is essential to prioritize your physical health after losing a patient. Nurses should get adequate sleep, eat healthy, and exercise regularly to maintain their physical well-being. In addition, some Nurses find that meditating or practicing yoga can help heal the mind and body.
Take a Break
Death is an emotional experience, and as Nurses, we are only human. It is not unreasonable to feel all the emotions surrounding the loss of a patient. It is OK to take a break when things get tough. If you are overwhelmed with emotions after losing a patient on the job, it’s ok to take a break to cry, take a walk, or call a friend to talk. It is important to care for your personal needs so you can get back to taking the best care of your patients.
Coping with the loss of a patient can be challenging, but the first step in learning to cope is acknowledging that grief is a normal reaction to any loss. Acknowledging your feelings, seeking support, practicing self-care, and knowing when you need to take a break can help prevent Nurses from experiencing burnout and get you back to providing your patients with excellent patient care.


 Congratulations on starting your Nursing career! Here are some pieces of advice that may help you as a new Nurse:
Congratulations on starting your Nursing career! Here are some pieces of advice that may help you as a new Nurse: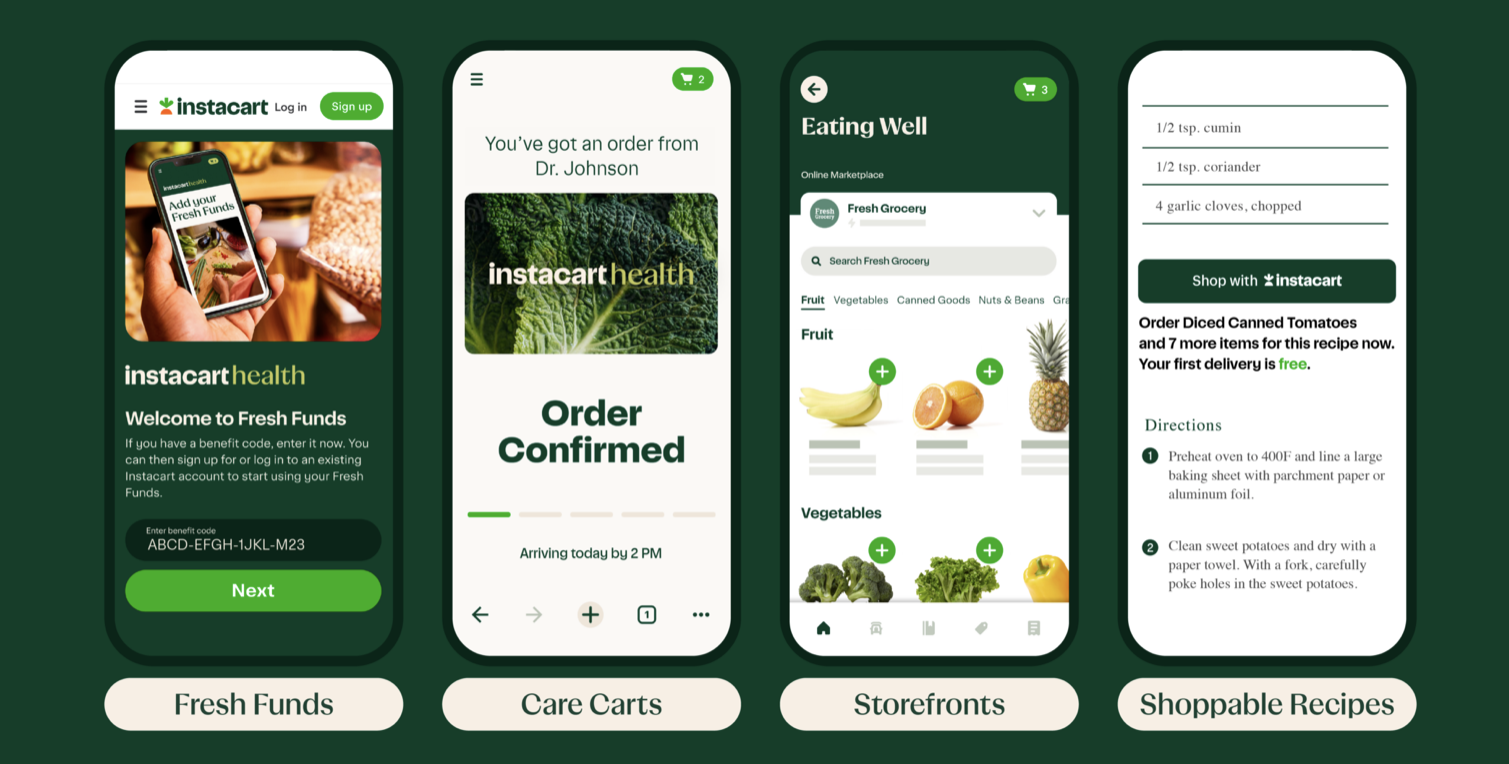 Healthcare providers recognize the crucial role nutritious diets play in promoting and maintaining good health. People with healthy eating patterns
Healthcare providers recognize the crucial role nutritious diets play in promoting and maintaining good health. People with healthy eating patterns  Patients become difficult for many different reasons. They sometimes become challenging due to diseases that affect their reasoning, like dementia or Alzheimer’s. Other times, patients can become verbally or physically abusive due to high-stress situations or unmet wants or needs. Regardless of why some patients become difficult, Nurses can help handle and diffuse difficult patient interactions with these 5 helpful tips.
Patients become difficult for many different reasons. They sometimes become challenging due to diseases that affect their reasoning, like dementia or Alzheimer’s. Other times, patients can become verbally or physically abusive due to high-stress situations or unmet wants or needs. Regardless of why some patients become difficult, Nurses can help handle and diffuse difficult patient interactions with these 5 helpful tips.  Choosing the right Nursing specialty can be a challenging decision, as there are many areas of Nursing to consider. Here are some steps that can help you choose the right specialty:
Choosing the right Nursing specialty can be a challenging decision, as there are many areas of Nursing to consider. Here are some steps that can help you choose the right specialty: Using humor in Nursing can be a valuable tool for creating a positive patient experience, improving communication, and reducing stress and anxiety among patients and fellow healthcare providers.
Using humor in Nursing can be a valuable tool for creating a positive patient experience, improving communication, and reducing stress and anxiety among patients and fellow healthcare providers. Hiring Nurses who reflect Diversity, Equity, and Inclusion (DEI) is an important step towards creating a healthcare system that is accessible and welcoming to all patients, regardless of their race, ethnicity, gender identity, sexual orientation, or any other characteristic.
Hiring Nurses who reflect Diversity, Equity, and Inclusion (DEI) is an important step towards creating a healthcare system that is accessible and welcoming to all patients, regardless of their race, ethnicity, gender identity, sexual orientation, or any other characteristic. 
 Emergencies can happen anywhere and patients need to be transported to facilities via ambulance or flight. This is when
Emergencies can happen anywhere and patients need to be transported to facilities via ambulance or flight. This is when 