 This article was written by the MODERN NURSE at www.discovernursing.com
This article was written by the MODERN NURSE at www.discovernursing.com
Nurses are the largest group of healthcare providers and you have a lot of power. You can help make changes that affect your patients and the environment. With climate change on the rise, you can create awareness of areas within your place of employment that need improvement. The reduction of strong chemicals, plastics and paper items can have a strong impact. Check out this interview regarding the Nursing community and how you can affect environmental change.
Public awareness and interest in all things “green” has created a need for nurses to understand environmental issues and their relationship to health with credible, evidence-based information, as well as provide leadership in making the necessary changes in our policies and practices. Cara Cook, MS, RN, AHN-BC, is working to increase awareness and promote action that addresses climate change as a health imperative among the nursing community through her role as climate change program coordinator for the Alliance of Nurses for Healthy Environments (ANHE). We spoke with Cara, who was recently chosen as a 2017 Johnson & Johnson Global Citizen Young Health Leader, about the connection between environmentalism and nursing, and how her background as a nurse has prepared her for advocacy work.
Nursing Notes (NN): How long have you been a nurse, and what significant changes have you seen in the nursing profession since you began practicing?
Cara: I’ve been a nurse for a little more than eight years, and one major change I’ve noticed is the nursing contribution to environmentally safe practice environments. Nurses have long been advocates for safe nurse-patient ratios and preventing adverse health outcomes, such as falls or healthcare-associated infections. In addition to those important patient safety issues, nurses are realizing the connection between the environments in which we live, work, and play, and how this influences health outcomes.
Nurses are at the forefront of change within practicing settings through advocating for use of safer chemicals in hospital cleaning supplies, by forming green teams or sustainability departments that focus on reducing an institution’s environmental impact, or from working in communities to ensure patients have access to healthy foods and safe areas to exercise.
NN: Why is understanding climate change important for nurses?
Cara: Climate change is one of the biggest global health threats we face today. Nurses are on the frontlines of communities caring for patients impacted by climate change, so it’s important for nurses to understand the connection between climate change and health, and how the health sector can respond.
As the most trusted profession and largest group of healthcare providers, nurses are urgently needed to lead the fight against climate change. Being aware of and advocating for solutions to limit and respond to climate change is within our scope of nursing practice, with our own practice standards stating the “registered nurse practices in an environmentally safe and healthy manner.”
NN: How did you get involved with ANHE?
Cara: As part of my master’s program, I was required to complete a certain number of hours for two semesters with a public health organization. Since my area of interest is in environmental health, I was paired to work with Katie Huffling, the executive director at ANHE. At that time, my work with ANHE involved federal reform of toxic chemical policy and participation in campaigns at the state level focused on advancing health-protective regulations for hydraulic fracturing and antibiotic use in animal agriculture. About a year after I graduated, ANHE received funding to expand their climate change and health program, and I came on board as a full-time employee.
NN: How has your background as a nurse prepared you for your current position?
Cara: Nurses feel very comfortable advocating on behalf of patients in healthcare facilities, so all it took was learning how to translate that skill into the policy arena. Another core part of nursing that has prepared me for my current position is the focus on evidence-based practice. Environmental health or climate change work is similar in that you need to look at the evidence in order to understand the issues and potential solutions, and how to adequately communicate this to the public or legislators.
Also, I think being able to work through the unanticipated and creatively solve problems when everything seems to be going wrong, as so often is needed in bedside nursing, has helped with working through some of the challenges in environmental health work.
NN: What do your day-to-day responsibilities look like as a climate change program coordinator?
Cara: My role includes spearheading ANHE’s climate change and health program that aims to increase awareness among the nursing profession on the health impacts posed by climate change. Through this program, I work to engage individual nurses and nursing organizations in prioritizing climate change as a health imperative, emphasizing the urgency for nursing action in frontline communities and in an advocacy role. One of our current initiatives is working to form a Nursing Collaborative on Climate Change and Health, which is an effort to unite national nursing organizations around climate change, with the goals of bringing health to the forefront of discussion and policy-making and ensuring a coordinated nursing response across specialties.
Since our organization has a small staff, I also help with our other environmental health initiatives, currently focused on water and health, air pollution, energy and health, safer chemicals, and food sustainability. ANHE also provides advocacy trainings, which I help organize and run, for nurses to learn how to be successful advocates on environmental health issues.
NN: What is your favorite part of your job?
Cara: My favorite part of my job is working with and meeting such amazing nurses. Working for ANHE allows me to meet and work with a variety of nurses from different specialties and learn more about the work being done to address environmental health issues. I lead ANHE’s Global Nurses Climate Change Committee, which provides an opportunity to connect with nurses across the world and learn about what is being done in other countries around climate change.
Another perk of my job is being able to talk with nurses about climate and health, and help them learn how they can move action forward in their own practice. It’s rewarding to inspire nurses to take action and to see how passionate they become when they learn about how climate change is creating significant challenges for health.
NN: What is the most challenging part of your job?
Cara: With environmental health work, and even policy work in general, it can be challenging not to get discouraged. Working with such a strong group of nurses helps to keep the momentum going when efforts can be disheartening.
NN: Looking forward, what advancements/changes do you expect to see in nursing?
Cara: Our healthcare system is in a fragile state, and there must be some dramatic changes for the system to be sustainable. We are already seeing a shift to prevention and building up the primary care system, with increasing attention to how environmental factors can affect health, and I think nurses and nurse practitioners will have a major role in this shift as our profession branches off into different avenues of care outside of traditional settings.
NN: Is there anything else that you would like to add?
Cara: Many of these environmental health issues, including climate change, can seem so daunting, almost as if there is nothing that can be done to reverse the course of action. However, there are solutions to address these complex issues and we are at a critical point where, as nurses we can make a big impact on the health of our patients and communities. Nurses are so important to moving the health message forward on climate change and, collectively, we have incredible power to drive change.
To learn more about environmental health and how climate change impacts health, or to join ANHE, visit envirn.org. For more information on Health Policy Nursing, visit DiscoverNursing.com. To learn more about the Johnson & Johnson partnership with Global Citizen, visit jnj.com/progress.






 Research has documented a number of
Research has documented a number of 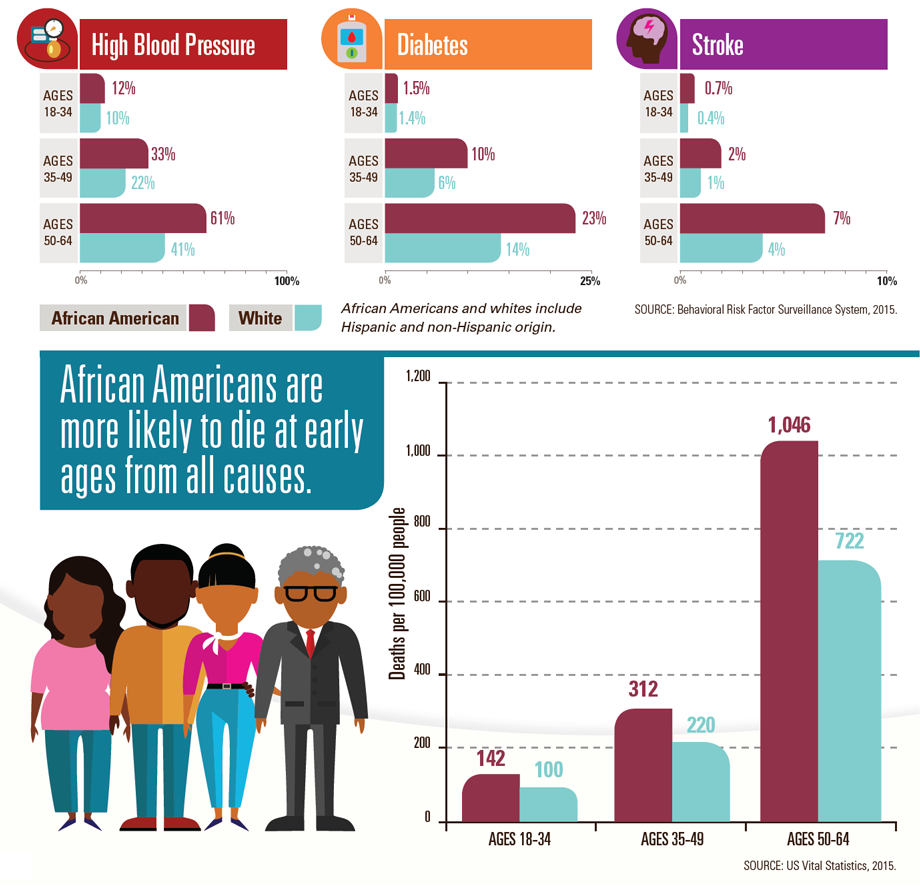
 ProPublica and NPR launched a project about maternal deaths and near-deaths in the U.S. In recent months, mothers who nearly died in the hours and days after giving birth have repeatedly
ProPublica and NPR launched a project about maternal deaths and near-deaths in the U.S. In recent months, mothers who nearly died in the hours and days after giving birth have repeatedly 
 “Example is not the main thing in influencing others. It is the only thing.”
“Example is not the main thing in influencing others. It is the only thing.”


 You might be a recent graduate and are worried about what to do when you get a difficult patient or maybe you are an experienced Nurse and are looking for new tips or ideas to try. We created a list of ways Nurses avoid or diffuse challenging situations with patients.
You might be a recent graduate and are worried about what to do when you get a difficult patient or maybe you are an experienced Nurse and are looking for new tips or ideas to try. We created a list of ways Nurses avoid or diffuse challenging situations with patients.