There is a growing need for more Nurse Educators to address the current shortage of Nurses and ensure the future generations of Nurses are well-trained and prepared to provide quality care.
There is a growing need for more Nurse Educators to address the current shortage of Nurses and ensure the future generations of Nurses are well-trained and prepared to provide quality care.
According to the Bureau of Labor Statistics’ Employment Projections 2021-2031, the Registered Nursing (RN) workforce is expected to grow by 6% over the next decade. The RN workforce is expected to grow from 3.1 million in 2021 to 3.3 million in 2031, an increase of 195,400 Nurses. The Bureau also projects 203,200 openings for RNs each year through 2031 when Nurse retirements and workforce exits are factored into the number of Nurses needed in the U.S.
The Advanced Practice Registered Nurse (APRN) workforce, including Nurse Practitioners, Nurse Anesthetists, and Nurse Midwives, is expected to grow much faster than average for all occupation, by 40% from 2021 through 2031, according to the BLS’ Occupational Outlook Handbook. Approximately 30,200 new APRNs, which are prepared in master’s and doctoral programs, will be needed each year through 2031 to meet the rising demand for care.
Nurse Educators play a vital role in the education and training of Nursing students and are responsible for developing and delivering curriculum, designing and implementing clinical experiences, and evaluating student progress.
The shortage of Nurse Educators at Nursing schools across the country are limiting student capacity at a time when the need for Nurses continues to grow.
According to the American Association of Colleges of Nursing (AACN), budget constraints, an aging faculty, and increasing job competition from clinical sites have contributed to this crisis.
However, increasing the number of Nurse Educators is critical to addressing the Nursing shortage and ensuring that there are enough qualified Nurses to meet the needs of patients.
There are several strategies that can be implemented to increase the number of Nurse Educators:
Increase Funding
Providing increased funding for Nursing education programs can help schools hire additional faculty and offer competitive salaries and benefits packages.
It's recommended, Congress pass legislation that would invest in Nursing faculty, clinical placements, and Nursing program facilities so that colleges and universities have the resources to enroll and graduate more students.
Tuition Forgiveness
Providing tuition forgiveness or loan repayment programs for Nurses who pursue advanced degrees in Nursing education can help incentivize Nurses to become Educators. Learn more about loan forgiveness or loan repayment programs here.
Mentorship Programs
Providing mentorship programs to support new Nurse Educators can help with their retention and success in the field. These programs are meant to encourage mutual professional growth between both the mentor and the mentee through a dynamic and supportive relationship.
Flexible Scheduling
People everywhere are demanding a shift toward work-life balance. Healthcare professionals are constantly working long hours, with little to no flexibility in their schedules. Offering flexible scheduling options can help attract individuals who may be interested in teaching but have other commitments, such as family or outside work.
Professional Development
Nurse Educators are tasked with nurturing the growth and education of Nurses, but they also need opportunities for growth and development. Offering opportunities for ongoing professional development, such as attending conferences or pursuing advanced degrees, can help keep Nurse Educators up-to-date on the latest Nursing practices and research.
Collaborations with Healthcare Facilities
Partnerships between Nursing schools and healthcare facilities can help provide clinical experiences for Nursing students and provide opportunities for Nurses to transition into teaching roles.
Katie Boston-Leary, PhD, RN, Director of Nursing programs at the American Nurses Association, told Becker's Hospital Review, she views it as "building a bridge" between schools and hospitals to train Nurses in real-world healthcare situations. Additionally, she said, growing an in-house team of Nurse Educators provides a pipeline for hospitals who can be actively involved in cultivating their own future workforces.
By implementing these strategies, Nursing schools and healthcare organizations can work together to address the shortage of Nurse Educators and make sure future generations of Nurses receive the education and training they need to provide high-quality patient care.



 Across the entire patient experience, Nurses have a hand in almost every aspect of the patient's healthcare journey. Nurses are compassionate, and dedicated, and work tirelessly to meet the needs of their patients. Because Nurses are at the forefront of every patient interaction, there are many things that we wish our patients knew and understood about how we work and handle our everyday tasks.
Across the entire patient experience, Nurses have a hand in almost every aspect of the patient's healthcare journey. Nurses are compassionate, and dedicated, and work tirelessly to meet the needs of their patients. Because Nurses are at the forefront of every patient interaction, there are many things that we wish our patients knew and understood about how we work and handle our everyday tasks.  A career as a Nurse Case Manager gives you the opportunity to make a huge impact on patient's lives and develop rewarding relationships.
A career as a Nurse Case Manager gives you the opportunity to make a huge impact on patient's lives and develop rewarding relationships. 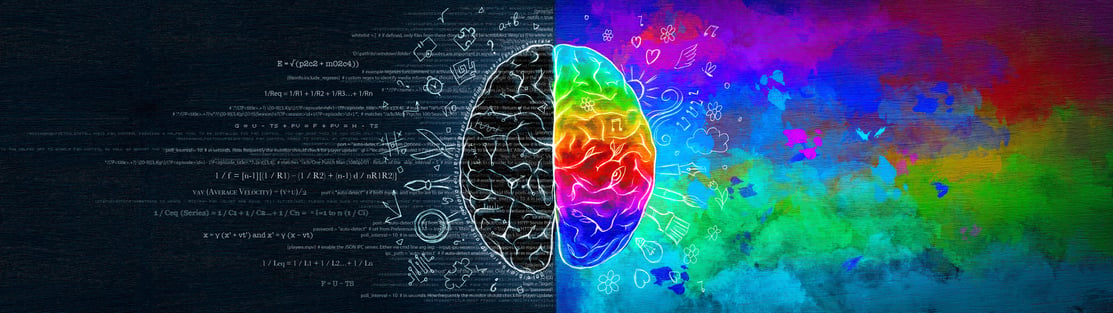 Nursing is a profession that requires compassion as well as expertise, making it both an art and a science. Empathy and compassion are critical characteristics of an excellent Nurse. These qualities help us to connect with patients on an individualized basis and improve patient outcomes.
Nursing is a profession that requires compassion as well as expertise, making it both an art and a science. Empathy and compassion are critical characteristics of an excellent Nurse. These qualities help us to connect with patients on an individualized basis and improve patient outcomes. 
 Even before the start of the COVID-19 Pandemic, it was well-known that the U.S. was facing a health care provider shortage. This trend was verified in a June 2020 report by the Association of American Medical Colleges^, which estimated the U.S. faces a potential physician shortage of 37,800 to 124,000 by 2034.
Even before the start of the COVID-19 Pandemic, it was well-known that the U.S. was facing a health care provider shortage. This trend was verified in a June 2020 report by the Association of American Medical Colleges^, which estimated the U.S. faces a potential physician shortage of 37,800 to 124,000 by 2034.  Health care organizations rely on Nurse leaders to manage teams, patient care, and promote organizational goals. In order to meet these goals, a successful Nurse leader must possess certain qualities such as...
Health care organizations rely on Nurse leaders to manage teams, patient care, and promote organizational goals. In order to meet these goals, a successful Nurse leader must possess certain qualities such as...