 The Nursing field offers many Nursing specialties to choose from depending on your interests and skills. And, there are plenty of opportunities to get the necessary training to move on to a different specialty.
The Nursing field offers many Nursing specialties to choose from depending on your interests and skills. And, there are plenty of opportunities to get the necessary training to move on to a different specialty.
The stress of the pandemic has increased Nurses' interest in positions beyond the hospital setting.
Some of those opportunities include:
Nurse Educator
Nurse Educators don’t work in a traditional hospital or medical facility. They teach in universities, technical schools, and hospital-based Nursing programs. They can also work as administrators, consultants, or independent contractors.
Forensic Nurse
According to ForensicNurses.org, Forensic Nurses provide specialized care for patients who are experiencing acute and long-term health consequences associated with victimization or violence, and/or have unmet evidentiary needs relative to having been victimized or accused of victimization. In addition, Forensic Nurses provide consultation and testimony for civil and criminal proceedings relative to Nursing practice, care given, and opinions rendered regarding findings.
Many Forensic Nurses work in hospitals but they also work in community anti-violence programs, coroner’s and medical examiners offices, corrections institutions, and psychiatric facilities.
Health Policy Nurse
A Health Policy Nurse (HPN) plays an active role in forming and communicating public health policies with the goal of improving the overall well-being of society. With a strong background of hands-on Nursing expertise, HPNs are able to aid and act as policy makers within our government and healthcare systems, according to Johnson & Johnson Nursing.
Flight Nurse
Flight Nurses provide care onboard medical helicopters, airplanes, or jets often used in emergency situations to get patients to the best hospital as quickly as possible.
Flight Nurses also transfer patients between facilities. Patients might need to be moved to obtain lifesaving treatment unavailable at the original facility or to relocate to another part of the country. They also communicate with medical professionals at the receiving facility, to ensure all case notes and patient files get to the right person.
Nurse Writer
Nurse writers educate readers on healthcare topics through their personal knowledge and experience.
According to RegisteredNursing.org, they can freelance for medical journals, guides, and other health-related publications (newspapers, magazines, websites, etc.) that require accumulated knowledge, education, experience, and objectivity. Nurses can also write academic papers, write grants for hospitals or programs, coordinate programs, or assist the Communications Department in hospitals or other organizations.
Camp Nurse
Camp Nurses typically serve children or teens, in a camp environment. This can include summer camps or other camps that last from days to weeks to even months at a time, but are usually temporary.
Depending on the size of the camp, Nurses could be required to work alone or as part of a team, making critical decisions on patient care. They may also be required to obtain and keep records on allergies, medical histories, and medications of all camp participants.
Dialysis Nurse
Dialysis Nurses work with patients suffering from kidney diseases and illnesses. They administer dialysis to patients at dialysis centers, nursing homes, or at the patient's home.
Yacht Nurse
As a Nurse/Stewardess, you will be expected to maintain the on-board medical ward and Nursing station. This includes overseeing stock inventory, ordering supplies, and recording inventories. Depending on the yacht owner's health, you may be required for certain medical duties.
Although long working hours are required, the benefits are amazing with salaries often higher than other Nursing positions. Yachting is not for the faint-hearted though and you must have a sense of adventure and an urge to travel.
A Nursing career isn't always a straight path. You have the opportunity to work in a variety of different environments and grow your skills and knowledge. Take a chance and use that degree to explore your options. Discover what Nursing path fulfills and challenges you.


 Even before the pandemic, healthcare providers experienced burnout and other negative mental health issues. Now more than ever, it is critical health systems take steps to support their staff's well-being.
Even before the pandemic, healthcare providers experienced burnout and other negative mental health issues. Now more than ever, it is critical health systems take steps to support their staff's well-being.

 It's no secret Nursing is a stressful and physically demanding career. H
It's no secret Nursing is a stressful and physically demanding career. H
 As the U.S. population becomes more racially and culturally diverse, having a workforce that mirrors the diversity of your community can improve the quality of care offered at your facility.
As the U.S. population becomes more racially and culturally diverse, having a workforce that mirrors the diversity of your community can improve the quality of care offered at your facility. Nursing is one of the most highly respected careers, but also one of the most stressful. This kind of stress can lead to compassion fatigue.
Nursing is one of the most highly respected careers, but also one of the most stressful. This kind of stress can lead to compassion fatigue. 
 Health care organizations rely on Nurse leaders to manage teams, patient care, and promote organizational goals. In order to meet these goals, a successful Nurse leader must possess certain qualities such as...
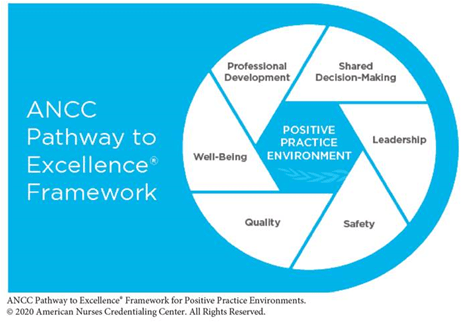
Health care organizations rely on Nurse leaders to manage teams, patient care, and promote organizational goals. In order to meet these goals, a successful Nurse leader must possess certain qualities such as... The culture of a work place can be described as the vibe of the environment, the day to day experience of staff and patients, and the way practices are implemented and followed.
The culture of a work place can be described as the vibe of the environment, the day to day experience of staff and patients, and the way practices are implemented and followed.